Uploaded by
common.user8914
Angle-closure glaucoma case in oculo-dento-digital syndrome
advertisement

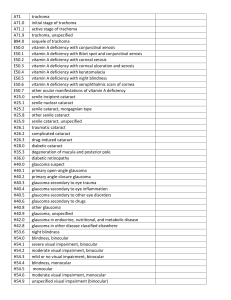
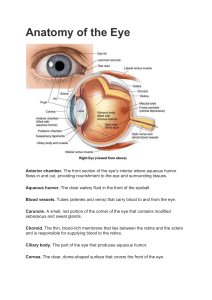
Graefe’s Arch Clin Exp Ophthalmol (2003) 241:161–163 S H O R T C O M M U N I C AT I O N DOI 10.1007/s00417-002-0619-z Randolf A. Widder Bert Engels Maria Severin Richard Brunner Günter K. Krieglstein Received: 18 February 2002 Revised: 14 November 2002 Accepted: 20 November 2002 Published online: 25 January 2003 © Springer-Verlag 2003 R. A. Widder (✉) · B. Engels M. Severin · R. Brunner · G. K. Krieglstein Zentrum für Augenheilkunde der Universität zu Köln, 50924 Cologne, Germany e-mail: [email protected] Tel.: +49-221-4786044 Fax: +49-221-4784347 A case of angle-closure glaucoma, cataract, nanophthalmos and spherophakia in oculo-dento-digital syndrome Abstract Background: We report a new case of oculo-dento-digital syndrome. Methods: Case report. Results: We saw a 34-year-old women with oculo-dento-digital syndrome. Visual acuity was no perception of light (RE) and 1/35 (LE). Biomicroscopy revealed a flat anterior chamber and an advanced cataract. The intraocular pressure (IOP) was 60 mmHg in both eyes. Ultrasonographic biomicroscopy demonstrated a closed chamber angle in both eyes. Measurements of the axial length and of the diameter of the lens were 18.7 mm/6.0 mm for the RE and 18.7 mm/5.8 mm for the LE respectively. In the time following we conducted a cyclodestructive procedure in the RE and a cataract extraction with implantation of an intraocular lens in the LE. This led to a considerable reduction of the IOP in the RE and combined with local therapy to IOP regulation in the LE. Conclusion: In this patient nanophthalmos, cataract and spherophakia led to angle-closure glaucoma in both eyes. We recommend early monitoring of IOP, axial length and lens diameter. This case demonstrates that an early cataract extraction might beneficially influence the natural course of the disease. Introduction Case report Oculo-dento-digital syndrome or Meyer-Schwickerath– Weyers syndrome is a rare disease which was first described as a clinical entity by Meyer-Schwickerath, Grüterich and Weyers in 1957 [8]. They stressed three features their four patients had in common. The main feature was microphthalmos. Other features were syndactyly of the fourth and fifth fingers and defects of dental enamel. All patients showed a striking unique appearance with small nasal alae and anteverted nostrils. The occurrence of glaucoma is known but the mechanisms show a heterogeneous pattern. In the literature patients with open-angle glaucoma, angle-closure glaucoma and chamber angle dysplasia are described [1, 5, 8, 12, 13]. Little is known about the natural course in patients with glaucoma. A 34-year-old women was referred to our department with the diagnosis of oculo-dento-digital syndrome and glaucoma. She complained about a deterioration of visual acuity in the past 2 years. Her face showed the typical appearance of oculo-dento-digital syndrome with small nasal alae and anteverted nostrils (Fig. 1). In her youth she had undergone surgery for syndactylies of the 4th and 5th fingers (Fig. 2). Her teeth had been extracted because of enamel dysplasia. She revealed a normal body shape, and other features such as complete epicanthal folds or skeletal changes were not noted. Visual acuity was perception of light in the right eye and 1/35 in the left eye. The corneal diameter was 6 mm in both eyes. Slit-lamp examination revealed a flat anterior chamber, a closed chamber angle and an advanced cataract. The intraocular pressure (IOP) was 50/45 mmHg under local therapy with miotic eye drops while the optic nerve head showed a pale appearance with a deep glaucomatous cupping. Ultrasonographic biomicroscopy (50 MHz, UBM 840, Zeiss-Humphrey) demonstrated a closed chamber angle in both eyes as well as a hypoplastic ciliary body (Fig. 3). Measurements of the axial length and of the diameter of the lens were 18.7 mm/6.0 mm for the right eye and 18.7 mm/5.8 mm for the left eye. For personal reasons the patient could not be hospitalized. Two months later we saw her again with 162 Fig. 3 Ultrasonographic biomicroscopy demonstrated a closed chamber angle in both eyes as well as a hypoplastic ciliary body Fig. 1 The typical appearance of oculo-dento-digital syndrome with small nasal alae and anteverted nostrils Fig. 2 In her youth the patient had undergone surgery for syndactylies of the 4th and 5th fingers an IOP of 60 mmHg in both eyes and no perception of light in the right eye. We then conducted a cyclodestructive procedure in the right eye, assuming that the procedure would trigger an IOP reduction despite the atrophic ciliary body. In the left eye a cataract extraction with implantation of an intraocular lens (Morcher Type 65C, Stuttgart; sulcus fixation) was performed. This led to a considerable reduction of the IOP in the right eye and was combined with local therapy for IOP regulation in the left eye. Discussion In view of the typical appearance of our patient and the presence of microphthalmos, syndactylies of the forth and fifth fingers and dental dysplasia we assigned the diagnosis of oculo-dento-digital syndrome [1]. About 50 individual cases are described in the literature as well as 42 members of a single family in eastern Europe [1, 5, 9, 13]. These cases were reported by various medical specialties and therefore the description of the patients with regard to ophthalmological features is incomplete. Oculo-dento-digital syndrome is regarded as an inherited disorder in an autosomal dominant fashion with variable expression. Additionally a high rate of de novo mutations is observed [4]. Our patient denied any affection of her relatives, but the family data were incomplete. 163 Meyer-Schwickerath and coworkers reported microphthalmos as the main feature of the disease as indicated by the title of their report: microphthalmos syndromes. However it remains unclear whether the patients show microcornea or microphthalmos. The axial eye length was rarely measured in the published studies and when recorded ranged from 20.8 to 26.2 mm. The interpretation of these findings is difficult because of the high variation in equipment and in measurement methods in different laboratories. In the seven patients whose axial eye length was measured there were no values below 20 mm was found but some of them might be considered as nanophthalmic eyes [1, 3, 5, 10]. No additional data describing the lens diameter are known. Our measurements suggest a nanophthalmic eye with spherophakia in our patient. A hypertrophy of the ciliary body with subsequent relaxation of the zonules is discussed as the cause of spherophakia [6, 8]. However, ultrasonographic biomicroscopy revealed a hypoplastic ciliary body in our patient. A hypoplastic ciliary body was also found by Dietlein and coworkers using ultrasonographic biomicroscopy in a patient with brachydactyly and spherophakia [2]. These and our findings may fit well with the observations of Vogt, who interpreted spherophakia as a sequela of incomplete development of the ciliary body. He postulated that the fetal lens remains in its spherical shape through a lack of tension. Glaucoma is often mentioned as a characteristic feature of oculo-dento-digital syndrome and follows a heterogeneous pattern, including trabeculodysgenesis-related glaucoma, open-angle glaucoma and angle-closure glaucoma [4, 13]. The latter was described by Sugar in two patients, and Meyer-Schwickerath and coworkers also mentioned a patient with a narrow chamber angle and highly elevated IOP. Measurement of IOP in patients with microcornea leads to various problems using Goldmann applanation or Schiötz tonometry. To achieve exact values an intraocular IOP measurement device seems necessary. In our patient, however, the highly elevated pressure was obvious. Goldmann and Schiötz tonometry were in the same range and fitted the estimates gained by digital evaluation. In our patient a closed chamber angle was seen at slit-lamp examination and ultrasonographic biomicroscopy. Probably the critical lens–eye length ratio led to a flattening of the anterior chamber with anterior synechiae and closure of the chamber angle [12]. Therefore we recommend early monitoring of IOP, axial length and lens diameter in these patients. In view of the difficulty of obtaining reliable IOP measurements in these patients, functional and morphological parameters such as optic disc cupping have to be given careful consideration. This case demonstrates that an early cataract extraction might beneficially influence the natural course of the disease, which, as seen in our patient’s other eye, can be devastating. References 1. Braun M, Seitz B, Naumann GOH (1996) Juveniles Offenwinkelglaukom mit Mikrocornea bei okulo-dento-digitaler Dysplasie (Meyer-SchwickerathWeyers). Klin Monatsbl Augenheilkd 208:262–263 2. Dietlein TS, Mietz H, Jacobi PC, Krieglstein GK (1996) Spherophakia, nanophthalmia, hypoplastic ciliary body and glaucoma in brachydactylyassociated syndromes. Graefes Arch Clin Exp Ophthalmol 234:187– 192 3. Dudgeon J, Chisholm IA (1974) Oculo-dento-digital dysplasia. Trans Ophthalmol Soc UK 94:203– 210 4. Gladwin A, Donnai D, Metcalfe K, Schrander-Stumpel C, Brueton L, Verloes A, Aylsworth A, Toriello H, Winter R, Dixon M (1997) Localization of a gene for oculodentodigital syndrome to human chromosome 6q22-q24. Hum Mol Genet 6:123–127 5. Judisch GF, Aurelio MC, Hanson JW, Olin WH (1979) Oculodentodigital dysplasia. Four new reports and a literature review. Arch Ophthalmol 97:878–884 6. Marchesani O (1939) Brachydaktylie und angeborene Kugellinse als Systemerkrankung. Klin Monatsbl Augenheilkd 103:392–406 7. Meyer SJ, Holstein T (1941) Spherophakia with glaucoma and brachydactyly. Am J Ophthalmol 24:247–257 8. Meyer-Schwickerath G, Grüterich E, Weyers H (1957) Mikrophthalmussyndrome. Klin Monatsbl Augenheilkd 131:18–30 9. Novotny L, Sterbova S (1984) MeyerSchwickerath Syndrom mit Mikrophthalmus. Klin Monatsbl Augenheilkd 185:282–285 10. Pfeiffer RA, Erpenstein H, Junemann G (1968) Oculo-dento-digitale Dysplasie. Klin Monatsbl Augenheilkd 152:247–262 11. Ritch R, Wand M (1981) Treatment of the Weil-Marchesani syndrome. Ann Ophthalmol 13:665–667 12. Sugar HS (1978) Oculodentodigital dysplasia syndrome with angle-closure glaucoma. Am J Ophthalmol 86:36–38 13. Traboulsi EI, Parks MM (1990) Glaucoma in oculo-dento-osseous dysplasia. Am J Ophthalmol 109:310–313