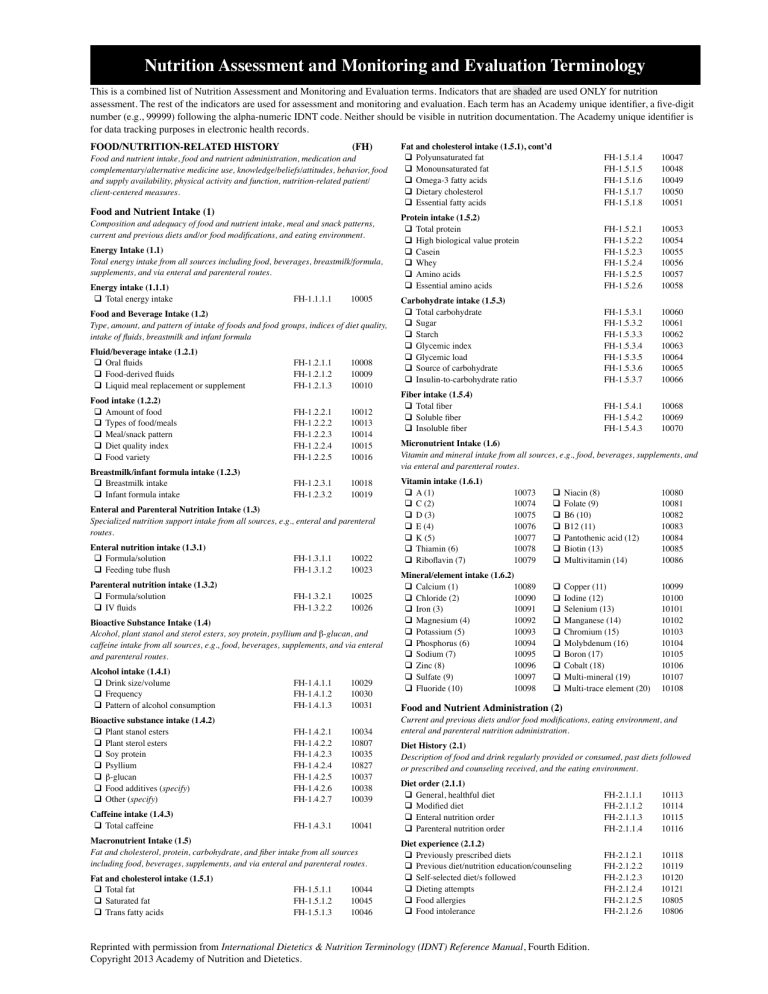
Nutrition Assessment and Monitoring and Evaluation Terminology This is a combined list of Nutrition Assessment and Monitoring and Evaluation terms. Indicators that are shaded are used ONLY for nutrition assessment. The rest of the indicators are used for assessment and monitoring and evaluation. Each term has an Academy unique identifier, a five-digit number (e.g., 99999) following the alpha-numeric IDNT code. Neither should be visible in nutrition documentation. The Academy unique identifier is for data tracking purposes in electronic health records. FOOD/NUTRITION-Related HISTORY (FH) Food and nutrient intake, food and nutrient administration, medication and complementary/alternative medicine use, knowledge/beliefs/attitudes, behavior, food and supply availability, physical activity and function, nutrition-related patient/ client-centered measures. Food and Nutrient Intake (1) Composition and adequacy of food and nutrient intake, meal and snack patterns, current and previous diets and/or food modifications, and eating environment. Energy Intake (1.1) Total energy intake from all sources including food, beverages, breastmilk/formula, supplements, and via enteral and parenteral routes. Energy intake (1.1.1) q Total energy intake FH-1.1.1.1 10005 Fluid/beverage intake (1.2.1) q Oral fluids q Food-derived fluids q Liquid meal replacement or supplement FH-1.2.1.1 FH-1.2.1.2 FH-1.2.1.3 10008 10009 10010 FH-1.2.2.1 FH-1.2.2.2 FH-1.2.2.3 FH-1.2.2.4 FH-1.2.2.5 10012 10013 10014 10015 10016 FH-1.2.3.1 FH-1.2.3.2 10018 10019 FH-1.3.1.1 FH-1.3.1.2 10022 10023 FH-1.3.2.1 FH-1.3.2.2 10025 10026 FH-1.4.1.1 FH-1.4.1.2 FH-1.4.1.3 10029 10030 10031 FH-1.4.2.1 FH-1.4.2.2 FH-1.4.2.3 FH-1.4.2.4 FH-1.4.2.5 FH-1.4.2.6 FH-1.4.2.7 10034 10807 10035 10827 10037 10038 10039 FH-1.4.3.1 10041 Food and Beverage Intake (1.2) Type, amount, and pattern of intake of foods and food groups, indices of diet quality, intake of fluids, breastmilk and infant formula Food intake (1.2.2) q Amount of food q Types of food/meals q Meal/snack pattern q Diet quality index q Food variety Breastmilk/infant formula intake (1.2.3) q Breastmilk intake q Infant formula intake Enteral and Parenteral Nutrition Intake (1.3) Specialized nutrition support intake from all sources, e.g., enteral and parenteral routes. Enteral nutrition intake (1.3.1) q Formula/solution q Feeding tube flush Parenteral nutrition intake (1.3.2) q Formula/solution q IV fluids Bioactive Substance Intake (1.4) Alcohol, plant stanol and sterol esters, soy protein, psyllium and b-glucan, and caffeine intake from all sources, e.g., food, beverages, supplements, and via enteral and parenteral routes. Alcohol intake (1.4.1) q Drink size/volume q Frequency q Pattern of alcohol consumption Bioactive substance intake (1.4.2) q Plant stanol esters q Plant sterol esters q Soy protein q Psyllium q b-glucan q Food additives (specify) q Other (specify) Caffeine intake (1.4.3) q Total caffeine Macronutrient Intake (1.5) Fat and cholesterol, protein, carbohydrate, and fiber intake from all sources including food, beverages, supplements, and via enteral and parenteral routes. Fat and cholesterol intake (1.5.1) q Total fat q Saturated fat q Trans fatty acids FH-1.5.1.1 FH-1.5.1.2 FH-1.5.1.3 10044 10045 10046 Fat and cholesterol intake (1.5.1), cont’d q Polyunsaturated fat q Monounsaturated fat q Omega-3 fatty acids q Dietary cholesterol q Essential fatty acids Protein intake (1.5.2) q Total protein q High biological value protein q Casein q Whey q Amino acids q Essential amino acids Carbohydrate intake (1.5.3) q Total carbohydrate q Sugar q Starch q Glycemic index q Glycemic load q Source of carbohydrate q Insulin-to-carbohydrate ratio Fiber intake (1.5.4) q Total fiber q Soluble fiber q Insoluble fiber FH-1.5.1.4 FH-1.5.1.5 FH-1.5.1.6 FH-1.5.1.7 FH-1.5.1.8 10047 10048 10049 10050 10051 FH-1.5.2.1 FH-1.5.2.2 FH-1.5.2.3 FH-1.5.2.4 FH-1.5.2.5 FH-1.5.2.6 10053 10054 10055 10056 10057 10058 FH-1.5.3.1 FH-1.5.3.2 FH-1.5.3.3 FH-1.5.3.4 FH-1.5.3.5 FH-1.5.3.6 FH-1.5.3.7 10060 10061 10062 10063 10064 10065 10066 FH-1.5.4.1 FH-1.5.4.2 FH-1.5.4.3 10068 10069 10070 Micronutrient Intake (1.6) Vitamin and mineral intake from all sources, e.g., food, beverages, supplements, and via enteral and parenteral routes. Vitamin intake (1.6.1) q A (1) q C (2) q D (3) q E (4) q K (5) q Thiamin (6) q Riboflavin (7) 10073 10074 10075 10076 10077 10078 10079 Mineral/element intake (1.6.2) q Calcium (1) 10089 q Chloride (2) 10090 q Iron (3) 10091 q Magnesium (4) 10092 q Potassium (5) 10093 q Phosphorus (6) 10094 q Sodium (7) 10095 q Zinc (8) 10096 q Sulfate (9) 10097 q Fluoride (10) 10098 q q q q q q q Niacin (8) Folate (9) B6 (10) B12 (11) Pantothenic acid (12) Biotin (13) Multivitamin (14) 10080 10081 10082 10083 10084 10085 10086 q q q q q q q q q q Copper (11) Iodine (12) Selenium (13) Manganese (14) Chromium (15) Molybdenum (16) Boron (17) Cobalt (18) Multi-mineral (19) Multi-trace element (20) 10099 10100 10101 10102 10103 10104 10105 10106 10107 10108 Food and Nutrient Administration (2) Current and previous diets and/or food modifications, eating environment, and enteral and parenteral nutrition administration. Diet History (2.1) Description of food and drink regularly provided or consumed, past diets followed or prescribed and counseling received, and the eating environment. Diet order (2.1.1) q General, healthful diet q Modified diet q Enteral nutrition order q Parenteral nutrition order Diet experience (2.1.2) q Previously prescribed diets q Previous diet/nutrition education/counseling q Self-selected diet/s followed q Dieting attempts q Food allergies q Food intolerance Reprinted with permission from International Dietetics & Nutrition Terminology (IDNT) Reference Manual, Fourth Edition. Copyright 2013 Academy of Nutrition and Dietetics. FH-2.1.1.1 FH-2.1.1.2 FH-2.1.1.3 FH-2.1.1.4 10113 10114 10115 10116 FH-2.1.2.1 FH-2.1.2.2 FH-2.1.2.3 FH-2.1.2.4 FH-2.1.2.5 FH-2.1.2.6 10118 10119 10120 10121 10805 10806 Nutrition Assessment and Monitoring and Evaluation Terminology, cont’d Eating environment (2.1.3) q Location q Atmosphere q Caregiver/companion q Appropriate breastfeeding accommodations/facility q Eats alone FH-2.1.3.1 FH-2.1.3.2 FH-2.1.3.3 FH-2.1.3.4 FH-2.1.3.5 Enteral and parenteral nutrition administration (2.1.4) q Enteral access FH-2.1.4.1 q Parenteral access FH-2.1.4.2 q Body position, EN FH-2.1.4.3 10123 10124 10125 10126 10127 10129 10130 10804 Medication and Complementary/Alternative Medicine Use (3) Prescription and over-the-counter medications, including herbal preparations and complementary/alternative medicine products used. Medications (3.1) q Prescription medication use q OTC medication use q Misuse of medication Complementary/Alternative Medicine (3.2) q Nutrtion-related complementary/alternative medicine use FH-3.1.1 FH-3.1.2 FH-3.1.3 10820 10134 10135 FH-3.2.1 10137 Knowledge/Beliefs/Attitudes (4) Understanding of nutrition-related concepts and conviction of the truth and feelings/ emotions toward some nutrition-related statement or phenomenon, along with readiness to change nutrition-related behaviors. Food and nutrition knowledge/skill (4.1) q Area(s) and level of knowledge/skill q Diagnosis specific or global nutrition-related knowledge score Beliefs and attitudes (4.2) q Conflict with personal/family value system q Distorted body image q End-of-life decisions q Motivation q Preoccupation with food/nutrients q Preoccupation with weight q Readiness to change nutrition-related behaviors q Self-efficacy q Self-talk/cognitions q Unrealistic nutrition-related goals q Unscientific beliefs/attitudes q Food preferences q Emotions Bingeing and purging behavior (5.3) q Binge eating behavior q Purging behavior Mealtime behavior (5.4) q Meal duration q Percent of meal time spent eating q Preference to drink rather than eat q Refusal to eat/chew q Spitting food out q Rumination q Patient/client/caregiver fatigue during feeding process resulting in inadequate intake 10180 10181 10182 FH-5.5.1 10184 Factors Affecting Access to Food and Food/Nutrition-Related Supplies (6) Factors that affect intake and availability of a sufficient quantity of safe, healthful food as well as food/nutrition-related supplies. Food/nutrition program participation (6.1) q Eligibility for government programs q Participation in government programs q Eligibility for community programs q Participation in community programs Safe food/meal availability (6.2) q Availability of shopping facilities q Procurement of safe food q Appropriate meal preparation facilities q Availability of safe food storage q Appropriate storage technique q Identification of safe food Safe water availability (6.3) q Availability of potable water q Appropriate water decontamination FH-6.1.1 FH-6.1.2 FH-6.1.3 FH-6.1.4 10187 10188 10189 10190 FH-6.2.1 FH-6.2.2 FH-6.2.3 FH-6.2.4 FH-6.2.5 FH-6.2.6 10192 10800 10194 10195 10196 10801 FH-6.3.1 FH-6.3.2 10198 10199 10848 10143 Food and nutrition-related supplies availability (6.4) q Access to food and nutrition-related supplies FH-6.4.1 q Access to assistive eating devices FH-6.4.2 q Access to assistive food preparation devices FH 6.4.3 FH-4.2.1 FH-4.2.2 FH-4.2.3 FH-4.2.4 FH-4.2.5 FH-4.2.6 FH-4.2.7 FH-4.2.8 FH-4.2.9 FH-4.2.10 FH-4.2.11 FH-4.2.12 FH-4.2.13 10145 10146 10147 10148 10149 10150 10151 10152 10153 10154 10155 10156 10157 Physical Activity and Function (7) Patient/client activities and actions, which influence achievement of nutrition-related goals. Avoidance behavior (5.2) q Avoidance q Restrictive eating q Cause of avoidance behavior Social network (5.5) q Ability to build and utilize social network FH-5.4.8 FH-5.4.9 FH-5.4.10 FH-4.1.1 FH-4.1.2 Behavior (5) Adherence (5.1) q Self-reported adherence score q Nutrition visit attendance q Ability to recall nutrition goals q Self-monitoring at agreed upon rate q Self-management as agreed upon Mealtime behavior (5.4), cont’d q Willingness to try new foods q Limited number of accepted foods q Rigid sensory preferences FH-5.1.1 FH-5.1.2 FH-5.1.3 FH-5.1.4 FH-5.1.5 10160 10161 10162 10163 10164 FH-5.2.1 FH-5.2.2 FH-5.2.3 10166 10167 10168 FH-5.3.1 FH-5.3.2 10170 10171 FH-5.4.1 FH-5.4.2 FH-5.4.3 FH-5.4.4 FH-5.4.5 FH-5.4.6 FH-5.4.7 10173 10174 10175 10176 10177 10178 10179 10201 10202 10203 Physical activity, cognitive and physical ability to engage in specific tasks, e.g., breastfeeding, self-feeding. Breastfeeding (7.1) q Initiation of breastfeeding q Duration of breastfeeding q Exclusive breastfeeding q Breastfeeding problems Nutrition-related ADLs and IADLs (7.2) q Physical ability to complete tasks for meal preparation q Physical ability to self-feed q Ability to position self in relation to plate q Receives assistance with intake q Ability to use adaptive eating devices q Cognitive ability to complete tasks for meal preparation q Remembers to eat q Recalls eating q Mini Mental State Examination Score q Nutrition-related activities of daily living (ADL) score q Nutrition-related instrumental activities of daily living (IADL) score Physical activity (7.3) q Physical activity history q Consistency q Frequency q Duration q Intensity q Type of physical activity q Strength q TV/screen time q Other sedentary activity time q Involuntary physical movement q NEAT FH-7.1.1 FH-7.1.2 FH-7.1.3 FH-7.1.4 10206 10207 10208 10209 FH-7.2.1 10211 FH-7.2.2 FH-7.2.3 FH 7.2.4 FH 7.2.5 FH-7.2.6 10212 10213 10214 10215 10216 FH-7.2.7 FH-7.2.8 FH-7.2.9 FH-7.2.10 10139 10218 10219 10220 FH-7.2.11 10221 FH-7.3.1 FH-7.3.2 FH-7.3.3 FH-7.3.4 FH-7.3.5 FH-7.3.6 FH-7.3.7 FH-7.3.8 FH-7.3.9 FH-7.3.10 FH-7.3.11 10223 10224 10225 10226 10227 10228 10229 10230 10231 10232 10233 Reprinted with permission from International Dietetics & Nutrition Terminology (IDNT) Reference Manual, Fourth Edition. Copyright 2013 Academy of Nutrition and Dietetics. Nutrition Assessment and Monitoring and Evaluation Terminology, cont’d Factors affecting access to physical activity (7.4) q Neighborhood safety q Walkability of neighborhood q Proximity to parks/green space q Access to physical activity facilities/programs FH-7.4.1 FH-7.4.2 FH-7.4.3 FH-7.4.4 10822 10823 10824 10825 Nutrition-Related Patient/Client-Centered Measures (8) Patient/client’s perception of his or her nutrition intervention and its impact on life. Nutrition quality of life (8.1) q Nutrition quality of life responses FH-8.1.1 Anthropometric Measurements 10236 (AD) Height, weight, body mass index (BMI), growth pattern indices/percentile ranks, and weight history. Body composition/growth/weight history (1.1) q Height/length q Weight q Frame size q Weight change q Body mass index q Growth pattern indices/percentile ranks q Body compartment estimates AD-1.1.1 AD-1.1.2 AD-1.1.3 AD-1.1.4 AD-1.1.5 AD-1.1.6 AD-1.1.7 Biochemical Data, Medical Tests and PROCEDURES 10239 10240 10241 10242 10243 10244 10245 (BD) Laboratory data, (e.g., electrolytes, glucose, and lipid panel) and tests (e.g., gastric emptying time, resting metabolic rate). Acid-base balance (1.1) q Arterial pH q Arterial bicarbonate q Partial pressure of carbon dioxide in arterial blood, PaCO2 q Partial pressure of oxygen in arterial blood, PaO2 q Venous pH q Venous bicarbonate Electrolyte and renal profile (1.2) q BUN q Creatinine q BUN:creatinine ratio q Glomerular filtration rate q Sodium q Chloride q Potassium q Magnesium q Calcium, serum q Calcium, ionized q Phosphorus q Serum osmolality q Parathyroid hormone Essential fatty acid profile (1.3) q Triene:Tetraene ratio Gastrointestinal profile (1.4) q Alkaline phosphatase q Alanine aminotransferase, ALT q Aspartate aminotransferase, AST q Gamma glutamyl transferase, GGT q Gastric residual volume q Bilirubin, total q Ammonia, serum q Toxicology report, including alcohol q Prothrombin time, PT q Partial thromboplastin time, PTT q INR (ratio) q Fecal fat q Amylase q Lipase q Other digestive enzymes (specify) q D-xylose q Hydrogen breath test q Intestinal biopsy q Stool culture BD-1.1.1 BD-1.1.2 BD-1.1.3 10248 10249 10250 BD-1.1.4 BD-1.1.5 BD-1.1.6 10251 10252 10253 BD-1.2.1 BD-1.2.2 BD-1.2.3 BD-1.2.4 BD-1.2.5 BD-1.2.6 BD-1.2.7 BD-1.2.8 BD-1.2.9 BD-1.2.10 BD-1.2.11 BD-1.2.12 BD-1.2.13 10255 10256 10257 10258 10259 10260 10261 10262 10263 10264 10265 10266 10267 BD-1.3.1 10269 BD-1.4.1 BD-1.4.2 BD-1.4.3 BD-1.4.4 BD-1.4.5 BD-1.4.6 BD-1.4.7 BD-1.4.8 BD-1.4.9 BD-1.4.10 BD-1.4.11 BD-1.4.12 BD-1.4.13 BD-1.4.14 BD-1.4.15 BD-1.4.16 BD-1.4.17 BD-1.4.18 BD-1.4.19 10271 10272 10273 10274 10275 10276 10277 10278 10279 10280 10281 10282 10283 10284 10285 10286 10287 10288 10289 Gastrointestinal profile (1.4), cont’d q Gastric emptying time q Small bowel transit time q Abdominal films q Swallow study Glucose/endocrine profile (1.5) q Glucose, fasting q Glucose, casual q HgbA1c q Preprandial capillary plasma glucose q Peak postprandial capillary plasma glucose q Glucose tolerance test q Cortisol level q IGF-binding protein q Thyroid function tests (TSH, T4, T3) q Pituitary hormone tests (GH, ACTH, LH, FSH) Inflammatory profile (1.6) q C-reactive protein Lipid profile (1.7) q Cholesterol, serum q Cholesterol, HDL q Cholesterol, LDL q Cholesterol, non-HDL q Total cholesterol:HDL cholesterol q LDL:HDL q Triglycerides, serum Metabolic rate profile (1.8) q Resting metabolic rate, measured q Respiratory quotient, measured Mineral profile (1.9) q Copper, serum or plasma q Iodine, urinary excretion q Zinc, serum or plasma q Boron, serum or plasma q Chromium, serum or urinary q Fluoride, plasma q Manganese, urinary, blood, plasma q Molybdenum, serum q Selenium, serum or urinary Nutritional anemia profile (1.10) q Hemoglobin q Hematocrit q Mean corpuscular volume q Red blood cell folate q Red cell distribution width q B12, serum q Methylmalonic acid, serum q Folate, serum q Homocysteine, serum q Ferritin, serum q Iron, serum q Total iron-binding capacity q Transferrin saturation Protein profile (1.11) q Albumin q Prealbumin q Transferrin q Phenylalanine, plasma q Tyrosine, plasma q Amino acid, other, specify q Antibody level, specify q Carbohydrate-deficient transferrin Urine profile (1.12) q Urine color q Urine osmolality q Urine specific gravity q Urine test, specify q Urine volume Reprinted with permission from International Dietetics & Nutrition Terminology (IDNT) Reference Manual, Fourth Edition. Copyright 2013 Academy of Nutrition and Dietetics. BD-1.4.20 BD-1.4.21 BD-1.4.22 BD-1.4.23 10290 10291 10292 10293 BD-1.5.1 BD-1.5.2 BD-1.5.3 BD-1.5.4 BD-1.5.5 BD-1.5.6 BD-1.5.7 BD-1.5.8 BD-1.5.9 BD-1.5.10 10295 10296 10297 10298 10299 10300 10301 10302 10303 10826 BD-1.6.1 10305 BD-1.7.1 BD-1.7.2 BD-1.7.3 BD-1.7.4 BD-1.7.5 BD-1.7.6 BD-1.7.7 10307 10308 10309 10310 10311 10312 10313 BD-1.8.1 BD-1.8.2 10315 10316 BD-1.9.1 BD-1.9.2 BD-1.9.3 BD-1.9.4 BD-1.9.5 BD-1.9.6 BD-1.9.7 BD-1.9.8 BD-1.9.9 10318 10319 10320 10841 10842 10843 10844 10845 10846 BD-1.10.1 BD-1.10.2 BD-1.10.3 BD-1.10.4 BD-1.10.5 BD-1.10.6 BD-1.10.7 BD-1.10.8 BD-1.10.9 BD-1.10.10 BD-1.10.11 BD-1.10.12 BD-1.10.13 10323 10324 10325 10326 10327 10328 10329 10330 10331 10332 10333 10334 10335 BD-1.11.1 BD-1.11.2 BD-1.11.3 BD-1.11.4 BD-1.11.5 BD-1.11.6 BD-1.11.7 BD-1.11.8 10337 10338 10339 10340 10341 10342 10343 10847 BD-1.12.1 BD-1.12.2 BD-1.12.3 BD-1.12.4 BD-1.12.5 10345 10346 10347 10348 10349 Nutrition Assessment and Monitoring and Evaluation Terminology, cont’d Vitamin profile (1.13) q Vitamin A, serum or plasma retinol q Vitamin C, plasma or serum q Vitamin D, 25-hydroxy q Vitamin E, plasma alpha-tocopherol q Thiamin, activity coefficient for erythrocyte transketolase activity q Riboflavin, activity coefficient for erythrocyte glutathione reductase activity q Niacin, urinary N’methyl-nicotinamide concentration q Vitamin B6, plasma or serum pyridoxal 5’phosphate concentration q Pantothenic acid, urinary pantothenate excretion, plasma q Biotin, urinary 3-hydroxyisovaleric acid excretion or lymphocyte propionyl-CoA carboxylase in pregnancy, serum BD-1.13.1 BD-1.13.2 BD-1.13.3 BD-1.13.4 BD-1.13.5 10351 10352 10353 10354 10355 BD-1.13.6 10356 BD-1.13.7 10357 BD-1.13.8 10358 BD-1.13.9 10850 BD-1.13.10 10851 Nutrition-Focused Physical Findings (PD) Findings from an evaluation of body systems, muscle and subcutaneous fat wasting, oral health, suck/swallow/breathe ability, appetite, and affect. Nutrition-focused physical findings (1.1) q Overall appearance (specify) ___________________________________ q Body language (specify) ___________________________________ q Cardiovascular-pulmonary (specify) ___________________________________ q Extremities, muscles and bones (specify) ___________________________________ q Digestive system (mouth to rectum) (specify) ___________________________________ q Head and eyes (specify) ___________________________________ q Nerves and cognition (specify) ___________________________________ q Skin (specify) ___________________________________ q Vital signs (specify) ___________________________________ PD-1.1.1 10362 PD-1.1.2 10363 PD-1.1.3 10364 PD-1.1.4 10365 PD-1.1.5 10366 PD-1.1.6 10367 PD-1.1.7 10368 PD-1.1.8 10369 PD-1.1.9 10370 Client History (CH) Current and past information related to personal, medical, family, and social history. Personal History (1) General patient/client information such as age, gender, race/ethnicity, language, education, and role in family. Personal data (1.1) q Age q Gender q Race/Ethnicity q Language q Literacy factors q Education q Role in family q Tobacco use q Physical disability q Mobility CH-1.1.1 CH-1.1.2 CH-1.1.3 CH-1.1.4 CH-1.1.5 CH-1.1.6 CH-1.1.7 CH-1.1.8 CH-1.1.9 CH-1.1.10 10374 10375 10376 10377 10378 10379 10380 10381 10382 10383 Patient/Client/Family Medical/Health History (2) Patient/client or family disease states, conditions, and illnesses that may have nutritional impact. Patient/client OR family nutrition-oriented medical/health history (2.1) Specify issue(s) and whether it is patient/client history (P) or family history (F) q Patient/client chief nutrition complaint CH-2.1.1 10386 (specify) __________________________________ P or F q Cardiovascular CH-2.1.2 10387 (specify) ___________________________________ P or F q Endocrine/metabolism CH-2.1.3 10388 (specify) ___________________________________ P or F q Excretory CH-2.1.4 10389 (specify) ___________________________________ P or F Patient/client OR family nutrition-oriented medical/health history (2.1), cont’d Specify issue(s) and whether it is patient/client history (P) or family history (F) q Gastrointestinal CH-2.1.5 10390 (specify) ___________________________________ P or F q Gynecological CH-2.1.6 10391 (specify) ___________________________________ P or F q Hematology/oncology CH-2.1.7 10392 (specify) ___________________________________ P or F q Immune (e.g., food allergies) CH-2.1.8 10393 (specify) ___________________________________ P or F q Integumentary CH-2.1.9 10394 (specify) ___________________________________ P or F q Musculoskeletal CH-2.1.10 10395 (specify) ___________________________________ P or F q Neurological CH-2.1.11 10396 (specify) ___________________________________ P or F q Psychological CH-2.1.12 10397 (specify) ___________________________________ P or F q Respiratory CH-2.1.13 10398 (specify) ___________________________________ P or F q Other CH-2.1.14 10399 (specify) ___________________________________ P or F Treatments/therapy (2.2) Documented medical or surgical treatments that may impact nutritional status of the patient q Medical treatment/therapy CH-2.2.1 10401 (specify) ___________________________________ q Surgical treatment CH-2.2.2 10402 (specify) ___________________________________ q Palliative/end-of-life care CH-2.2.3 10404 (specify) ___________________________________ Social History (3) Patient/client socioeconomic status, housing situation, medical care support and involvement in social groups. Social history (3.1) q Socioeconomic factors (specify) ___________________________________ q Living/housing situation (specify) ___________________________________ q Domestic issues (specify) ___________________________________ q Social and medical support (specify) ___________________________________ q Geographic location of home (specify) ___________________________________ q Occupation (specify) ___________________________________ q Religion (specify) ___________________________________ q History of recent crisis (specify) ___________________________________ q Daily stress level CH-3.1.1 10407 CH-3.1.2 10408 CH-3.1.3 10409 CH-3.1.4 10410 CH-3.1.5 10411 CH-3.1.6 10412 CH-3.1.7 10413 CH-3.1.8 10414 CH-3.1.9 10415 COMPARATIVE STANDARDS (CS) Energy Needs (1) Estimated energy needs (1.1) q Total energy estimated needs q Method for estimating needs CS-1.1.1 CS-1.1.2 10419 10420 CS-2.1.1 CS-2.1.2 CS-2.1.3 10423 10424 10425 CS-2.2.1 CS-2.2.2 CS-2.2.3 10427 10428 10429 Macronutrient Needs (2) Estimated fat needs (2.1) q Total fat estimated needs q Type of fat needed q Method for estimating needs Estimated protein needs (2.2) q Total protein estimated needs q Type of protein needed q Method for estimating needs Reprinted with permission from International Dietetics & Nutrition Terminology (IDNT) Reference Manual, Fourth Edition. Copyright 2013 Academy of Nutrition and Dietetics. Nutrition Assessment and Monitoring and Evaluation Terminology, cont’d Estimated carbohydrate needs (2.3) q Total carbohydrate estimated needs q Type of carbohydrate needed q Method for estimating needs Estimated fiber needs (2.4) q Total fiber estimated needs q Type of fiber needed q Method for estimating needs CS-2.3.1 CS-2.3.2 CS-2.3.3 10431 10432 10433 CS-2.4.1 CS-2.4.2 CS-2.4.3 10435 10436 10437 Estimated fluid needs (3.1) q Total fluid estimated needs q Method for estimating needs CS-3.1.1 CS-3.1.2 10440 10441 Fluid Needs (3) Micronutrient Needs (4) Estimated vitamin needs (4.1) q A (1) 10444 q C (2) 10445 q D (3) 10446 q E (4) 10447 q K (5) 10448 q Thiamin (6) 10449 q Riboflavin (7) 10450 q q q q q q q Niacin (8) Folate (9) B6 (10) B12 (11) Pantothenic acid (12) Biotin (13) Method for estimating needs (14) 10451 10452 10453 10454 10455 10456 10458 Estimated mineral needs (4.2) q Calcium (1) 10460 q Chloride (2) 10461 q Iron (3) 10462 q Magnesium (4) 10463 q Potassium (5) 10464 q Phosphorus (6) 10465 q Sodium (7) 10466 q Zinc (8) 10467 q Sulfate (9) 10469 q Fluoride (10) 10470 q q q q q q q q q Copper (11) Iodine (12) Selenium (13) Manganese (14) Chromium (15) Molybdenum (16) Boron (17) Cobalt (18) Method for estimating needs (19) 10471 10473 10474 10475 10476 10477 10478 10479 10480 Weight and Growth Recommendation (5) Recommended body weight/body mass Index/growth (5.1) q Ideal/reference body weight (IBW) CS-5.1.1 q Recommended body mass index (BMI) CS-5.1.2 q Desired growth pattern CS-5.1.3 Reprinted with permission from International Dietetics & Nutrition Terminology (IDNT) Reference Manual, Fourth Edition. Copyright 2013 Academy of Nutrition and Dietetics. 10483 10484 10485