Uploaded by
common.user65506
Medical Morning Report: September 1st, 2020 - Clinical Cases
advertisement

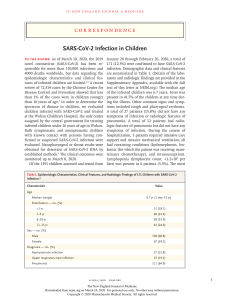
MORNING REPORT September, 1st 2020 PHYSICIAN IN CHARGE : IA : dr. Ros, dr. Dandi, dr. Jodi II Konsulan : dr. Pandu II HCU : dr. Angel INCOVIT Ward : dr. Farid II ER : dr. Yosi, dr. Reta INCOVIT ER : dr. Surya Chief : dr. Amanda Consultant : dr. Heri Sutanto, SpPD PROBLEM ORIENTED MEDICAL RECORD Cue and Clue P2 Incovit/ Mr. F/ 64 y.o (referral from PKM Tumpang) Primary survey : Circulation: warm, Airway: patent Breathing: spontan Secondary survey : Chief complaint : Fever • Fever since 7 day before admission, intermittently, relieved after he was given Paracetamol. Headache (+), malaise and nausea since a week. Cough and shortness of breath was denied. He was admitted at PKM Tumpang for 3 days and said to had dengue fever. • Lump in his neck since 20 years ago, and was planned to had surgery but he refused. He was diagnosed with hyperthyroidism and DM type 2 since 2 months ago, and routinely controlled to Endocrinology outpatient clinic. He took methimazole 1x20mg, acarbose 3x50mg, and metformin 3x500mg. • He lived in Poncokusumo, Tumpang, and work in a candle factory in Bululawang Objective : looked moderately ill; GCS 456; BP: 113/71 mmHg; PR: 102 bpm; RR: 18 tpm; Tax: 36,8°C (38,9C at PKM Tumpang); SaO2: 99% RA H/N : Struma uninodusa (+), size 6x9x4cm, bruit (-); Abd : flat, soefl, tenderness (-) ; Ext : warm +/+ edema -/Laboratory Finding 1/9/2020 CBC : 12/6.870/36,4%/177.000 MCV/MCH : 76,7/26,9 fl/pg Diff count : 0,3/0,3/75,8/17,0/6,6 NLR : 4,46; CRP 2,47 mg/d; SE : 136/4,26/112 mmol/L; OT/PT 41/51 U/L; Albumin : 3,33 g/dL Ur/Cr : 48/0,89 Procalcitonin 0,85 ng/mL Total Antibody SarsCov2 Non Reactive; RBG 203 mg/dl; T3/T4 2,51/2,82 ng/dl; TSH 0,04 uU/mL; Bil T/D/I 0,32/0,19/0,13 CXR 1/9/2020 Pneumonia possible viral causes Struma cervicothoracalis deviating the trachea to the right ECG 1/9/2020 Sinus rhytm HR 99 bpm BW Score : Heart rate +5; Precipitating event +10 = 15 (unlikely to represent thyroid storm Problem List and Initial Diagnosis Emergency: - Planning Urgency: - PDx Urinalysis, Naso+Oropharyngeal swab Non Urgency: 1. Struma uninodusa toxica 1.1 Toxic Adenoma 1.2 Thyroid Cyst 1.3 Ca thyroid 2. AFI day 7 (resolved) 2.1 Infection 2.1.1 Probable Covid-19 2.1.2 UTI 2.2 Related to impending thyroid storm 3. DM type 2 on OAD 4. Pneumonia probable Covid-19 5. Nausea 5.1 Related to no 2 PTx - Bedrest - Diet 1800 kcal/day - Rehidration NS 500cc continue by 1500cc/24h - IV Lansoprazole 1x30mg - IV Metoclopramide 3x10mg - IV Levofloxacine 1x750mg - PO Methimazole 1x20mg - PO Propranolol 3x20 mg - PO Acarbose 3x50mg - PO Metformin 3x500mg - PO Paracetamol 3x500mg - PO Zinc 3x20mg - PO Hydroxychloroquin 1x400mg PMo S, VS, BW score Patient was planned to admitted at Covid Ward (but the family refused) References: EIMED PAPDI War d Inco vit ER PROBLEM ORIENTED MEDICAL RECORD Cue and Clue Identity: P2/ Mrs. M/ 41 yo Primary survey : Circulation: warm, Airway: patent Breathing: spontan Secondary survey : Chief complaint : Headache - Headache since morning, pain like sharp and stabbing, worsened since afternoon, no weakness in half of the body (-) pelo (-) history of admission 1 month ago with the same complaint (+) - Nausea and vomiting once this afternoon, fill ed with residual food - Diagnosed with kidney failure since 1.5 years ago, routine dialysis twice a week (every Wednesday and Saturday) using AV Shunt access - HT (+) 2 years, routine consumption of captopril, clonidine, adalat oros consumption this afternoon, history of DM (-) Objective: GA: Looked moderately Ill, GCS: 4-5-6; BP: 217/ 116 -> 191/96 mmHg, PR: 82 bpm, RR: 20 tpm, Tax: 36,5°C, SaO2: 100% on RA VAS : 5/10 H/N: conj anemis (-/-) pupil isokhor 3 mm/3 mm Tho: P/ves/ves Rh-/Wh-/-C/ ict palpable @ 2cm lat ICS V MCL Sin Abd/flat, BU (+) N, soefl Ext/warm, edema (-/-) MMT 5/5/5/5 sensory within normal limit Laboratory Findings (01/09/2020) CBC 11,7 / 11,040 / 34,7% / 142,000 MCV/MCH 90,4/30,5 fl/pg Diff 0,5/0,2/78,8/14,9/5,6% TLC 1,650 NLR 5,27 RBS: 101 mg/dl albumin 4,8 mg/dl Ur/Cr: 123,8/ 15,33 mmol/L eGFR: 2,56 ml/min/m2 Na/K/Cl: 136 / 4,34 / 107 mmol/L Ca/Ph 10,3/4,9 mg/dl CRP 0,22 Procalcitonin 0,48 Antibodi Anti-SARS-COV2: Non Reaktif CXR : Cardiomegaly ECG : Sinus Rhytm HR 82 bpm, LVH Problem List and Initial Diagnosis Planning Emergency (-) Planning Diagnosis (-) Urgency 1. HT urgency Planning Therapy Nonpharmacology - Bedrest + proper position - Renal Diet 1800 kkal/day, low salt <2g/day, protein 1-1,2 g/kgBB/day Pharmacology - IV plug - IV Furosemide 3x20 mg - IV Metoclopramide 3x10 mg - Po Captopril 3x25 mg - Po Clonidine 3x0,15 ug - Po Nifedipin 3x10 mg - Po Paracetamol 3x1000 mg - HD elective as scheduled Non Urgency 2. CKD st 5 on routine HD 2.1 HT Nephrosclerosis 2.2 Glomerulonephritis chronic 2.3 IgA Nephropathy 3. Tension type Headache 3.1 Related to no.1 4. HF st C fc II 4.1 Hypertensive heart diseases 4.2 Uremic cardiomyopathy 4.3 CRS type 4 5. Nausea vomiting 5.1 Uremic gastropathy 5.2 PUD Planning Monitor - VS, UOP, VAS, target organ damage REFERENCE: EIMED, PAPDI