Uploaded by
nailahrahmah1997
Referat on Hyperthyroidism: Definition, Diagnosis, and Management
advertisement

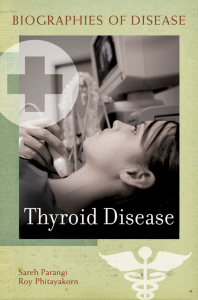
REFERAT HIPERTIROID Oleh : Nailah Rahmah (406181048) Pembimbing : dr. Eddy Mulyono, SpPD, FINASIM KEPANITERAAN ILMU PENYAKIT DALAM PERIODE 21 OKTOBER 2018 – 30 DESEMBER 2018 RUMAH SAKIT UMUM DAERAH RAA SOEWONDO PATI FAKULTAS KEDOKTERAN UNIVERSITAS TARUMANAGARA JAKARTA DEFINITION ▹ Clinical condition caused by increased synthesis and secretion of hormones by the thyroid gland which affects the entire body. ▹ Thyrotoxicosis is defined as clinical manifestations related to increased thyroid hormone levels ▹ Disease : Diffuse Toxic Goiter (Grave’s Disease), Toxic Multinodular Goiter, Toxic Adenoma, and Thyroid Storm EPIDEMIOLOGY ▹ Graves' disease (GD) persists as the most frequently-encountered etiology of hyperthyroidism causing approximately 60-80% of all cases of thyrotoxicosis worldwide. ▹ Female-to-male ratio of 8:1 and apparently manifests in the third and fourth decades of life. Thyroid nodules Medications Thyroiditis Causes Grave’s Disease Excessive iodine intake ROLE OF THYROID STIMULATING IMMUNOGLOBULIN IN GRAVES DISEASE SIGN AND SYMPTOMS OF HYPERTHYROIDSM Sign & Symptomps WAYNE’S INDEX OF SIGN AND SYMPTOMS IN DIAGNOSTIC APPROACH OF HYPERTHYROIDISM ALGORITHM FOR THE DIAGNOSTIC WORKUP OF HYPERTHYROIDISM CLINICAL EVALUATIONS ▹ Biochemical evaluation ▸ Overt hyperthyroidism is characterized by suppressed TSH (<0.01 mU/L) and excess thyroid hormones in serum. ▹ Serum TSH ▸ Highest sensitivity and specificity, used as an initial screening test for hyperthyroidism (TSH will be less than 0.01 mU/L or even undetectable) ▹ ▹ FT4 & T3 : To confirm the abnormal serum TSH TRAb (thyrotropin receptor antibody) ▸ This approach is utilized when a thyroid scan and uptake are unavailable or contraindicated (e.g., during pregnancy and lactation). THYROID FUNCTION TEST IN HYPERTHYROIDSM AND IN CONDITIONS STIMULATING HYPERTHYROIDISM DIAGNOSIS OF HYPERTHYROIDISM ▹ ▹ ▹ To distinguish between hyperthyroidism and other causes of thyrotoxicosis, a radioactive iodine uptake (RAIU) should be performed. Hyperthyroidism has high RAIU while the other etiologies have low or near absent radioactive iodine uptake. The assessment of hyperthyroidism manifestations, and especially potential cardiovascular and neuromuscular complications, is essential to formulating an appropriate treatment plan. CLINICAL EVALUATIONS Imaging ▹ Ultrasonography (USG) ▸ USG is performed with the patient in the supine position and the neck hyperextended. USG can detect thyroid lobes or lesions as small as 2 mm. It can distinguish solid nodules from simple and complex cysts. It can estimate thyroid size, give a rough estimate of tissue density, show vascular flow and velocity and aid in placing a needle for diagnostic purpose. Doppler studies may be added while executing ultrasonography. ▹ Fine needle aspiration biopsy (FNAB) ▸ In GD, FNAB is necessary if a nodule is found within the thyroid – to distinguish benign from malignant nodules which may occur. We recommend an USG-guided FNAB. MANAGEMENT 1. Inhibition of thyroid hormone synthesis and secretion (ATDs) 2. Destruction or reduction of thyroid tissue mass (radioactive iodine therapy or surgery) 3. Minimalization of thyroid hormone effects on peripheral tissues (beta-blocker therapy) PHARMACOLOGIC TREATMENT OF HYPERTYROIDSM PTU or Methimazol e DOC : PTU or MMI? – Although methimazole (MMI) and propylthiouracil (PTU) have long been used to treat hyperthyroidism caused by Graves’ disease (GD), there is still no clear conclusion about the choice of drug or appropriate initial doses – Journal : “Comparison of Methimazole and Propylthiouracil in Patients with Hyperthyroidism Caused by Graves’ Disease” Objectiv e Compare the MMI 30 mg/d treatment with the PTU 300 mg/d and MMI 15 mg/d treatment in terms of efficacy and adverse reactions. Patients Main Outcom e Measure s - 371 Patients newly diagnosed with GD were randomly assigned to one of the three treatment regimens in a prospective study at four Japanese hospitals. - Divided in 2 groups; Group A patients are those with pretreatment serum FT4 less than 7 ng/dl and group B with 7 ng/dl or more Percentages of patients with normal serum free T4 (FT4) or free T3 (FT3) and frequency of adverse effects were measured at 4, 8, and 12 wk RESULTS FT4 & FT3 • MMI 30 mg/d normalized FT4 & FT3 in more patients than PTU 300 mg/d and MMI 15 mg/d for the whole group (240 patients) at 12 wk Severe Hyperthyroidism • When patients were divided into two groups by initial FT4, in the group of the patients with severe hyperthyroidism (FT4, 7 ng/dl or more, 64 patients) MMI 30mg/d normalized FT4 more effectively than PTU 300mg/d at 8 and 12 wk and MMI 15mg/d at 8 wk, respectively Adverse Effects • Mild hepatotoxicity, were higher with PTU and significantly lower with MMI 15 mg/d compared with MMI 30 mg/d IS MMI SAFE FOR LONGTERM USE? – The major clinical problem of antithyroid therapy is the 20–70% relapse of hyperthyroidism following discontinuation of treatment – Journal : “Effect of long-term continuous methimazole treatment of hyperthyroidism: comparison with radioiodine” Results : Long-term continuous treatment of hyperthyroidism with MMI is safe. The complications and the expense of the treatment do not exceed those of radioactive iodine therapy Objectiv e To investigate the long-term methimazole (MMI) therapy Patients Main Outcom e Measure s effects of continuous - 504 patient with diffuse toxic goiter were treated with MMI for 18 months - Within one year after discontinuation of MMI, hyperthyroidism recurred in 104 patient - They were randomized into 2 groups for continuous antithyroid and radioiodine treatment - Numbers of occurrences of thyroid dysfunction and total costs of management were assessed during 10 years of follow-up Serum thyroid and lipid profiles, bone mineral density, and echocardiography data were obtained. Side Effects ▹ During 10 years of successive MMI treatment in the 26 patients of group 1, except for minor allergic symptoms, no serious complications, including agranulocytosis, occurred Results ▹ Nearly 10 years of follow-up of such patients showed that this mode of treatment is safe and its cost does not exceed that of radioiodine treatment ▹ At the end of 10 years, goiter rate was greater and antithyroperoxidase antibody concentration was higher in group 1 than in group 2 ▹ Serum cholesterol and low density lipoprotein-cholesterol concentrations were increased in group 2 as compared with group 1 ▹ Bone mineral density and echocardiographic measurements were not different between the two groups IS MMI SAFE FOR LONGTERM USE? – Journal : “Long-Term, Low-Dose Methimazole Reduces Hyperthyroidism Relaps” – Results : long-term low dose methimazole treatment for 60-120 months is a safe and effective method for treatment of Grave hyperthyroidism – Optimal duration : 12-18 month – Optimal dose : < 5 mg 302 Patients Treat with MMI for 18 mo 258 Selected randomly 130 128 Continue 115 Continue until 60 mo minimal (mean : 96 mo) Stop 15 Stop Results OCCURRENCE OF RELAPS 60 50 40 30 20 10 0 Results (%) While Follw-up (in 12 mo) (%) After Follow-up (48 mo) (%) Short-term Long-term Column1 Side Effects ▹ First 18 mo : no major complication; cutaneous reaction (14 patient), elevated of liver enzyms (2 patients) ▹ No side effects for long-term therapy Conclusions ▹ long-term low dose methimazole treatment for 60-120 months is a safe and effective method for treatment of Grave hyperthyroidism ▹ So these data are reassuring, suggesting that as long as patients are consistent wiyh taking the methimazole and don’t show signs of toxicity, longer-term reasonable strategy term is HOW ABOUT PTU? – From journal : “Long-term outcomes of patients with propylthiouracil-induced anti-neutrophil cytoplasmic auto-antibody-associated vasculitis” – ANCA-associated vasculitis (AAV) is associated with high morbidity and mortality, thus identification of potentially reversible causes of AAV, such as specific drugs, is very important – Propylthiouracil (PTU) is a common antithyroid drug, which has been known to induce AAV with multiple ANCA antigen specificity Results ▹ The long-term outcomes of patients with PTUinduced AAV were relatively good ▹ PTU should be discontinued immediately after diagnosis ▹ Immunosuppressive therapy may be only used in patients with vital organ involvements, and a longterm maintenance therapy may not be necessary Thank You