Uploaded by
common.user56313
Advanced Clinical Practitioner Job Description - Emergency Medicine
advertisement

CORE JOB DESCRIPTION
ADVANCED CLINICAL PRACTITIONER
JOB TITLE:
Advanced Clinical Practitioner in Emergency Medicine
BAND:
8A
BASE:
Your primary base will be Leicester Royal Infirmary, however
travel between UHL’s hospital sites will be required
HOURS:
37.5 hours per week internal rotation
REPORTS TO:
Lead ACP / Head of service
ACCOUNTABLE TO:
Chief Nurse
ABOUT UHL, OUR VALUES AND BEHAVIOURS
Every day at University Hospitals of Leicester we save lives, improve lives and usher in new life.
Our Trust Values determine our behaviour and our culture. We are a passionate and creative team
and at our best when we work together. Our Values are:
1.We treat people how we would like to be treated
2. We do what we say we are going to do
3. We focus on what matters most
4. We are one team and we are best when we work together
5. We are passionate and creative in our work
As one of the very largest NHS Trusts in the country, our contribution to our communities goes way
beyond direct health; we are the largest employer in our region, we educate and train the staff of
the future, we push research boundaries and with our £1bn turnover we are an economic engine
for the wider East Midlands and beyond.
This is particularly exciting time for Leicester’s Hospitals. We have been given £450m by the
Government to provide a host of new facilities and reconfigure services between our three main
sites. Flagship projects include a new Children’s Hospital, a new Maternity Hospital, a new
Treatment Centre and two new Intensive Care Units. Equally importantly, we are going
“paperless”, with a £12m investment in our NerveCentre computer system to help our team deliver
world class care.
1
We want to continue to improve everything that we do, so that we can achieve our Vision: Caring
at its best for every patient, every time. Our Quality Strategy, “Becoming the Best”, describes
how we are doing that in a determined, targeted and systematic way, with our staff the champions
of change and our patients not just beneficiaries but partners.
“Becoming the Best” is based on best practice from “outstanding” organisations within the NHS
and abroad. It has six key elements:
We understand what is happening in our services, so that we know what needs to be
improved
We have clear priorities and plans for improvement, so that we are clear about what we
are trying to do
We are developing our culture and leadership, so that everyone is empowered and
encouraged to make improvements
We have adopted a single approach to improvement (our quality
improvement methodology), and are giving people at all levels the skills to use it
We always involve our patients when we are making improvements that impact on them
and their care
We are integrating this work with the wider health and social care system, of which we
are a part.
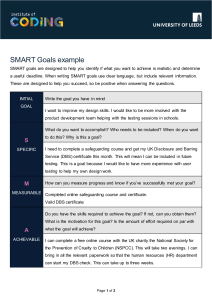
These elements are shown in the diagram below (the blue cog), together with the specific priorities
that we are working on at the moment (the pick and green cogs).
2
JOB DESCRIPTION
CORE JOB SUMMARY
The post holder will be an integral member of the medical team working collaboratively
with nursing and allied healthcare professionals undertaking advanced roles and
responsibilities traditionally the remit of junior medical staff under the direction of the
Consultant in charge of the patients care.
The Advanced Practitioner will work within agreed protocols and guidelines exercising
independent judgement in history taking, examination, assessment, diagnosis, and
treatment of a diverse and undetermined caseload of unwell medical and acutely ill
patients who may have highly complex acute presentation to the more minor common
illnesses.
The post will have a primary / location but may extend and influence across UHL, including
the Emergency Department and hospital wards.
The Advanced Practitioner will act as a professional resource for the multi professional
teams, patients and carers. They will ensure that evidence based practice is inherent in all
aspects of care and treatment and ensure this knowledge is disseminated throughout the
clinical area, across the Trust and externally as appropriate.
The Advanced Practitioner will triage referrals either independently or with medical /
therapy colleagues and make onward referrals in line with Trust policies.
KEY RESPONSIBILITIES
1.0
CLINICAL
1.1
To accept clinical responsibility for undertaking the comprehensive assessment of a
caseload of patients, including those with a complex presentation, in line with
evidence based practice, legislation, policies and procedures. Using investigative
and analytical skills; review and interpret all information available, utilising a
systematic process of reasoning to make a differential diagnosis.
1.2
Provide treatment plans for patients that are consistent with the outcome of
assessment and the most probable diagnosis using current clinical pathways where
required in order to facilitate timely, quality patient care and / or appropriate onward
referral.
1.3
Where appropriate, initiate diagnostic tests, interpret and act upon results and
provide advice to members of the multidisciplinary team on patient treatment.
Evaluates the effectiveness of interventions/treatments and makes any necessary
modification.
Practice autonomously; performing advanced practice skills that have been agreed
with the senior nursing and medical teams within the specialty.
1.4
3
1.5
To use an extended scope of practice beyond own profession recognising any
limitations in knowledge, referring to senior medical staff when scope of practice is
exceeded
1.6
Maintain a safe environment for patients, relatives and staff, and adhering to
infection prevention policies.
1.7
As a registered non-medical prescriber, independently prescribe medication and
fluids within current legislation and Trust policies.
1.8
To accept referrals from and make referrals to consultants, GPs, and other
healthcare professionals. Review the patient and act accordingly, thereby reducing
length of time patients wait for intervention.
1.9
Improve the quality of the patient experience by identifying and meeting the
individual clinical needs of patients. Act at all times in the patients best interests and
as a patient advocate.
1.10
Provide specialist advice on patient care to the healthcare team and act as a
specialist resource within the service and other areas within the Trust.
1.11
To maintain comprehensive and accurate assessment and treatment records
(written and electronic) in line with legal, professional and Trust requirements, and
communicate assessment and treatment results to the appropriate disciplines in the
form of letters and / or reports.
2.0
MANAGEMENT AND LEADERSHIP
2.1
Understands professional accountability and legal frameworks for advanced
practice
2.2
To be professionally accountable and legally responsible for all aspects of own
work, including the management of patients in your care.
2.3
Demonstrate safe practice in line with the Trust Quality, Safety and Risk
Management Policies, Child Protection and Safeguarding Vulnerable Adults
Policies, Consent and assent regulations and the UHL ‘Do Not Attempt
Resuscitation’ Policy.
2.4
Act as a role model in the clinical area, promoting and demonstrating the standards
of care and behaviours expected. Provide appropriate challenge to individuals when
required raising quality issues and related risks with relevant people and addressing
poor performance as per Trust policy (i.e. complaints and incidents, poor
communication with patients, relatives or staff).
2.5
Demonstrate and plan efficient and effective use of resources against the agreed
speciality or team budgets.
2.6
Contribute towards Ward / Department / Service or Trust meetings at which broad
professional and service issues are discussed.
4
2.7
Encourage and influence the multidisciplinary team to identify and discuss
opportunities to develop clinical practice, protocols, policies and guidance for the
speciality utilising current evidence and ensuring meaningful consultation, effective
evaluation and sharing of results.
2.8
Be proactive in developing own professional practice, demonstrating evidence of
increasing autonomy, clinical judgment and decision making skills whilst
contributing to the development of others.
3.0
EDUCATION AND TRAINING
3.1
Provide an authoritative and credible source of knowledge and specialist clinical
advice/information to the team by keeping abreast of new treatments and
technologies for the speciality.
3.2
Actively maintains self development, objectively reviewing own performance in
terms of management, clinical practice and decision making, identifying own needs
and taking steps to meet those needs.
3.3
Demonstrate responsibility for personal professional development using feedback
and reflection aligned to the NMC Code and maintain a Professional Portfolio to
improve personal clinical practice whilst meting the future requirements of
Revalidation of Nursing and Midwifery.
3.4
Participate in planning and delivery of multidisciplinary education programmes for
staff within speciality and wider arena to promote learning opportunities and the
development of clinical skills.
3.5
Provide supervision, support and training for student and foundation advanced
nurse practitioners enabling them to develop and apply their knowledge and skills in
practice. Provide timely feedback to individual practitioners and their line managers
to support this process, identifying, reporting and proactively dealing with poor
performance.
3.6
Participate in the development and delivery of specialist training programmes for
nursing and medical undergraduate students, student and foundation advanced
practitioners, post-registration nurses and other groups of learners, making effective
use of all learning opportunities developing the workplace as a learning
environment.
3.7
Be an active member of the continuing education, in-house programmes by the
attendance and presentation at staff meetings, tutorials, training sessions, journal
clubs, external courses, clinical supervision and reflective practice.
Undertakes annual mandatory training and ‘essential to job role’ updates and other
relevant courses in line with professional and Trust policies.
3.8
5
4.0
RESEARCH AND AUDIT
4.1
Participate in data collection for audit including research projects.
4.2
Participate in audit, mortality and morbidity and other clinical meetings where the
outcomes and recommendations have the potential to improve the quality of care,
give case presentations as required.
4.3
Identify areas of own clinical practice that require research/audit. Devise
audit/research tools, analyse data, write report and present findings to the
multidisciplinary team. Complete audit cycle by implementing change in practice as
required and re-auditing.
4.4
Research that has been undertaken should be disseminated both locally and
nationally at seminars, conferences and through publication in national journals.
4.5
Develop evidence based policies and procedures specifically required by the
specialty.
5.0
COMMUNICATION
5.1
Communicates effectively with a wide range of people in a manner consistent with
their level of understanding, culture and background and preferred ways of
understanding that meet mental or physical health needs e.g. altered conscious
level, sensory loss, altered perception, pain, fear, and severe psychosocial
problems; identifying and managing challenging behaviour .
5.2
To assess capacity, gain valid informed consent and have the ability to work within
a legal framework with patients who lack capacity to consent to treatment.
5.3
Demonstrates an empathetic and reassuring approach to communicating highly
sensitive condition related information and advice to patients, carers and relatives.
5.4
Competently receives highly sensitive information concerning patients medical
condition and acts appropriately
Health & Safety
Be aware of the Health and Safety aspects of your work and implement any policies which
may be required to improve the safety of your work area, including the prompt recording
and reporting of accidents to senior staff, and ensuring that equipment used is safe.
To comply with the organisational and departmental policies and procedures and to be
involved in the reviewing and updating as appropriate.
Monitors and maintains health, safety and security of self and others in own work area.
Identifies and assesses potential risks in work activities and proposes how to manage
these risks appropriately.
Contributes to the NHSLA risk register.
6
Works within legislation and Trust procedures on risk management.
Takes immediate and appropriate action in relation to adverse incident reporting utilising
the hospital incident reporting system.
You are accountable for the effective deployment of activities that ensure that your
department/ward/clinical team is reducing hospital acquired infection. You will ensure that
you and your staff comply with the Trust’s policies on infection, prevention and control.
You will ensure that you and your staff receive the training required to maintain
competence to execute the Trusts policies on infection, prevention and control. You have a
responsibility to bring deficiencies in the deployment of such policies to the attention of
your line manager.
Freedom to Act
The Advanced Nurse Practitioner will work without direct supervision as an autonomous
practitioner being accountable for own practise in line with the Nursing and Midwifery Code
guided by Trust protocols and interpreting national guidelines and policies applicable to
own sphere of practice.
To practice competently, you must possess the knowledge, skills and abilities required for
lawful, safe and effective practice without direct supervision. You must acknowledge the
limits of your professional competence and only undertake and accept responsibilities for
those activities in which you are competent including the safe use of medical equipment.
KEY RESPONSIBILITIES
The Advanced Care Practitioner will become a key member of a skilled multidisciplinary
team providing high quality assessment and intervention for patients on the Acute Medical
Unit including the Acute Care Bay
1. Undertake the day-to-day assessment and management of acutely ill adult patients.
Actively contribute to the daily ward rounds
2. Undertake a wide range of advanced clinical skills where appropriate training has
been complete and competency achieved.
These skills should include:
venepuncture, female and male catheterisation, arterial and central venous
cannulation, arterial blood gas sampling and interpretation of results requesting
investigations (such as blood test, ECG, CXR, and US) and interpretation of results
to support clinical management plans, and advanced life support during cardiac
arrests.
3. Where appropriate initiate diagnostic tests, interpret and act upon results and
provide advice to members of the multidisciplinary team on patient treatment. This
will include: requesting appropriate blood tests, arterial blood gas sampling and
interpretation of results, requesting and performing ECGs, requesting radiological
7
investigations (such as CXR, US, CT, and MRI) and interpretation of results to
support clinical management plans.
GENERAL
All employees are subject to the requirements of the Health & Safety at Work Act and
prevailing Acts since. It is the post-holders responsibility to ensure they are familiar with
all UHL Health and Safety related policies that apply to their workplace or work –practice.
The post holder is required to ensure that as an employee, his or her work methods do not
endanger other people or themselves.
All employees are subject to the requirements of the current Data Protection legislation
and must maintain strict confidentiality in respect of patient’s and staff’s records.
All employees must comply with the Trust’s Equal Opportunities Policy and in line with the
Equality Act 2010, must not discriminate on grounds of age, disability, gender
reassignment, race, religion or belief, marriage or civil partnership, pregnancy or maternity,
sexual orientation or sex. Other grounds on which they should not treat others
unfavourably include trade union membership (or non-membership) or political affiliation,
or any other grounds which cannot be shown to be justifiable.
This job description is not to be taken as an exhaustive list of duties and it may be
reviewed in the light of changed service needs and development. Any changes will be
fully discussed with the post holder. The post holder will be required to carry out the duties
appropriate to the grade and scope of the post.
The Trust is committed to supporting the health and wellbeing of all its employees. Should
the post holder be employed in a people management capacity then they will be required
to familiarise themselves with the organisation’s range of health and wellbeing support,
share with their team, and appropriately manage stress and ill health in accordance with
Trust policies, procedures, legislation and best practice.
In order to ensure the Trust’s ability to respond to changes in the needs of the service,
after appropriate consultation and discussion with you (including consideration of personal
circumstances current skills, abilities and career development) the Trust may make a
change to your location, duties and responsibilities that are deemed reasonable in the
circumstances.
Your normal place of work will be as discussed at interview and will be confirmed in
Section 1 of your contract but you may be required to work in other locations of the Trust.
In particular, flexibility is required across the three main Hospital sites (Leicester Royal
Infirmary, Leicester General Hospital, Glenfield Hospital). If your initial location is based at
one of these sites, excess travel reimbursement will not apply for a permanent/temporary
change to base.
8
Health Clearance for Healthcare Workers (‘Occupational Health checks’)
1) It is recommended that all new healthcare workers have checks for tuberculosis (TB)
disease/immunity and are offered hepatitis B immunisation (with post-immunisation
testing of response) and blood tests for evidence of infection with hepatitis C and HIV
[1]. Being free of infectious tuberculosis is mandatory. Checks for immunity to
measles, mumps, rubella and varicella (chicken pox) will also be made and vaccination
offered if immunity is not detected.
These standard health clearance checks will be completed on appointment. Managers
should inform new workers that they must contact the OH department so the necessary
arrangements can be made. Even if the new worker has had similar checks recently
elsewhere, or has worked in UHL before, they will still need to attend for a review,
unless these were undertaken at UHL as part of a current rotational medical
appointment.
2) For healthcare workers who will perform exposure-prone procedures (EPPs), work in a
renal unit*, or likely to practice in an exposure prone environment, additional health
clearance must be undertaken. Additional health clearance includes testing or
demonstration of satisfactory test results for:
HIV
Hepatitis B
Hepatitis C
The exact standards that must be met are described in detail in the Public Health England
document: Integrated guidance on health clearance of healthcare workers and the
management of healthcare workers infected with blood borne viruses (hepatitis B, hepatitis
C and HIV) October 2017, or revisions thereof.
*Workers in renal units only need to demonstrate satisfactory results for Hepatitis B.
These additional checks should be completed before confirmation of an appointment to an
applicable post, as the healthcare worker will be ineligible if they do not meet the required
criteria. Those who refuse to have the required tests will not be given clearance to start
work.
All tests will be arranged in confidence through the Occupational Health department. All
costs for testing will be borne by the employing organisation.
[1] Health clearance for tuberculosis, hepatitis B, hepatitis C and HIV: New
healthcare workers. DoH 2007.
9
DISCLOSURE AND BARRING SERVICE (DBS) –
{Formerly known as Criminal Records Bureau (CRB)}
If this post requires a standard/enhanced disclosure by the DBS, it is regulated by statute.
Failure to disclose details if you are currently / or in the future the subject of police
investigation / proceedings which could result in a conviction, caution, bind over order or
charges is a disciplinary matter, and may result in dismissal.
The cost of undertaking a DBS disclosure at the required level and associated
processing costs will be met by the individual.
To expedite the process the Trust will meet the initial costs of the disclosure which
will be deducted from the individuals’ salary over a three month period commencing
on their first months payment.
INFECTION CONTROL
Registered Healthcare Professionals
All healthcare professionals on a professional register are personally accountable for their
standards of practice which must include compliance with the Trust’s infection prevention
and control policies and guidelines. In addition all registered practitioners are expected to
challenge non-compliance when observed to protect patients and promote patient safety.
Local clinical leaders have a responsibility to maintain an organisational culture of
vigilance through their role in supervising other staff.
SAFEGUARDING CHILDREN AND VULNERABLE ADULTS
The post holder is responsible for safeguarding the interests of children and adults who
they come into contact with during their work. To fulfil these duties post holders are
required to attend training and development to recognise the signs and symptoms of
abuse or individuals at risk, to follow local and national policy relating a safeguarding
practice and to report and act on concerns that they may have.
RESPONSIBILITIES
DEVELOPMENT
FOR
CONTINUING
EDUCATION
AND
PERSONAL
Undertake the Trust Corporate and Directorate specific Induction and competency
Programmes appropriate to role.
LEADERSHIP AND COMMUNICATION
If you are in a leadership position and are invited to attend the monthly Chief Executive’s
Briefing, you are required to attend one of the briefing sessions. You are then required to
10
meet with your team to cascade the information received and to subsequently provide
feedback on your team’s discussions.
ELECTRONIC ROSTERING
Our Electronic Rostering system is key to ensuring staff are in the right place with the right
skills at the right time, to ensure we carry out this responsibility effectively; all UHL staff
must adhere to the rostering standards and guidelines set out in the Electronic Rostering
Policy, pertaining to their role.
Statement On The Recruitment Of Ex-Offenders
As an organisation using the Disclosure and Barring Service (DBS) to assess applicants’
suitability for positions of trust, the University Hospitals of Leicester NHS Trust complies
fully with the DBS Code of Practice and undertakes to treat all applicants for positions
fairly. It undertakes not to discriminate unfairly against any subject of a Disclosure on the
basis of conviction or other information revealed.
The University Hospitals of Leicester NHS Trust is committed to the fair treatment of its
staff, potential staff or users of its services, regardless of race, gender, religion, sexual
orientation, responsibilities for dependants, age, physical/mental disability or offending
background.
We actively promote equality of opportunity for all with the right mix of talent, skills and
potential and welcome applications from a wide range of candidates, including those with
criminal records. We select all candidates for interview and appointment based on their
skills, qualifications and experience.
A Disclosure is only requested after a thorough risk assessment has indicated that one is
both proportionate and relevant to the position concerned. For those positions where a
Disclosure is required, job adverts and job descriptions will contain a statement that a
Disclosure will be requested in the event of the individual being offered the position.
Where a Disclosure is to form part of the recruitment process, we encourage all applicants
called for interview to provide details of their criminal record at an early stage in the
application process. At interview, or in a separate discussion, we ensure that an open and
measured discussion takes place on the subject of any offences or other matter that might
be relevant to the position. At conditional offer stage, we ask applicants to complete a
declaration form. This is only seen by those who need to see it as part of the recruitment
process.
Unless the nature of the position allows the University Hospitals of Leicester NHS Trust to
ask questions about your entire criminal record we only ask about “unspent” convictions as
defined in the Rehabilitation of Offenders Act 1974. Failure to reveal information that is
directly relevant to the position sought could lead to withdrawal of an offer of employment.
We will discuss any matter revealed in a Disclosure with the person seeking the position
should a situation arise where we are required to withdrawal conditional offer of
11
employment. We have a specialist team who is available on hand to provide support and
guidance on these matters.
There is a DBS Code of Practice details of which
https://www.gov.uk/government/publications/dbs-code-of-practice
are
available
Having a criminal record will not necessarily bar you from working with us. This will
depend on the nature of the position and the circumstances and background of your
offences.
12
at:
CORE PERSON SPECIFICATION
Post: Advanced Nurse Practitioner
Band: 8A
CMG / DIRECTORATE: Emergency and Specialist Medicine
Criteria
Essential
Commitment to Trust
Values and Behaviours
Must be able to demonstrate
behaviours consistent with the
Trust’s Values and Behaviours
Registered professional with no
restrictions on practice.
NMC/HCPC
MSc Advanced Clinical Practice
or equivalent
Recognised Teaching &
Assessing Qualification
Research module / qualification
Registered Independent NonMedical Prescriber
ALS/APLS
ETC
Education &
Qualifications
Desirable
13
Stage Measured at
A – application
I – Interview
T – Test
Interview
Application
Study at level 8
ALS/APLS instructor
NMC Pin Check
University certification
NMC Register
Advanced clinical skills
Evidence of advanced skills in
history taking and physical
examination skills
Highly developed communication
skills
Ability to assess, diagnose and
action under pressurised
environments
Demonstrates expertise in
complex decision making.
Ability to provide Strong
Inspirational leadership
Able to deliver
Coaching/facilitation skills
Ability to support Staff
development and empowerment
Ability to influence service
changes
Influence standard setting
Speciality Module - MBChB 1,
equivalent to 6 months study
– medical school anatomy
MBChB 2, equivalent to 7
weeks study with 4th year
medical students
Evidence of performing minor
surgical procedures
Experience
Lead in Research projects
Highly developed specialist
experience and knowledge in
the speciality of the post being
applied for
Autonomous management of
own patient load (ward based or
clinic environment)
Autonomously assess, diagnose
and develop management plans
for urgently referred patients
14
Application form
Interview presentation
Communication and
relationship skills
Equality and Diversity
2 years in Emergency medicine
as practitioner
Band 7 with knowledge and skills
that can be accredited or mapped
against the essential criteria of
this role
Extensive clinical experience
In depth specialist knowledge
Evidence of the application of
management/leadership skills and
autonomous practice
Experience of audit
Experience in teaching specialist
skills and knowledge
Experience in Research and
development
Experience of service
development
Organisational and negotiation
skills
Effective communicator in
complex situations
Leadership and motivation skills
Self motivated.
Able to facilitate change.
Able to lead and work within a
team
Ability to motivate others.
Able to demonstrate a
commitment and understanding
15
Application form
Interview presentation
Interview
Other requirements
specific to the role
of the importance of treating all
individuals with dignity and
respect appropriate to their
individual needs.
Ability to work on own initiative
and within a team.
Vision to develop the service and
the role of the ANP.
Awareness of the East Midlands
Advanced Practice Framework
Ability to formulate long term
strategic plans to develop service
across the organisation
16
Application form
Interview.