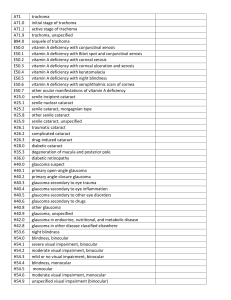
Chlamydia Conjunctivitis Chlamydia Conjunctivitis Is caused by Chlamydia Trachomatis bacteria Devide into 3 types: 1. Trachoma: serotypes A–C 2. Adult and neonatal inclusion conjunctivitis: serotypes D–K 3. lymphogranuloma venereum: serotypes L1, L2, and L3 Trachoma • Trachoma is an infectious disease that occurs in communities with poor hygiene and inadequate sanitation. • It affects approximately 150 million individuals worldwide and is the leading cause of preventable blindness. • Transmission may also occur by flies and household fomites, • Trachoma typically begins in childhood as a bilateral chronic follicular conjunctivitis that due to recurrent episodes progresses to conjunctival scarring Trachoma Symptoms and Signs: Foreign-body sensation, redness, tearing, and mucopurulent discharge. Clinical diagnosis of trachoma requires at least 2 of the following clinical features: 1. 2. 3. 4. 1 Follicles on the tarsal conjunctiva (usually upper tarsal) Limbal follicles and their sequelae (Herbert pits) HALLMARK OF TRACHOMA Typical tarsal conjunctival scarring Vascular pannus most marked on the superior limbus 2 3 4 Trachoma WHO made a simple severity grading for other trained personnel other than ophthalmologists based on the presence or absence of 5 key signs: 1. Follicular conjunctival inflammation 2. Diffuse conjunctival inflammation 3. Tarsal conjunctival scarring 4. Aberrant lashes 5. Corneal opacification Trachoma Management: WHO made SAFE' strategy for the management of trachoma. • S: Surgery for Trichiasis and Ectropion • A: Antibiotics for C. trachomatis infection • tetracy- cline 1% ophthalmic ointment, applied twice daily for 2 months, and oral azithromycin 1000 mg, given as a single dose. • Oral erythromycin is recommended for treat- ment of rare tetracyclineresistant cases. • F: Facial cleanliness • E: Environmental change to improve sanitation and increase access to clean water. Adult and neonatal inclusion conjunctivitis • a sexually transmitted disease often found in conjunction with chlamydial urethritis or cervicitis. Mode transmission: 1. Direct/Indirect contact with infected genital secretions. (newborn and sexually active transmission) 2. Shared eye cosmetics 3. Inadequately chlorinated swimming pools Adult and neonatal inclusion conjunctivitis Symptoms and Sign: Adult Newborn • Local: Papillae and follicles especially in lower tarsus. Scant mucopurulent discharge Superficial Keratitis superiorly. Palpable preauricular adenopathy. Small Micropannus No pseudomembrane • Local: papillary conjunctivitis, a moderate amount of exudate, and in hyperacute casespseudomembranes occasionally form and can lead to scarring. • < 3 months: no follicle formation • > 3 months: follicles appear , WHY ? • Systemic: Otitis media • Systemic: pharyngitis, otitis media, and interstitial pneumonitis. Adult and neonatal inclusion conjunctivitis • Laboratory Finding: • Enzyme Immunosorbent Assay (ELISA) • PCR • Direct fluorescent antibody test- use for newborn to prevent systemic complication • How to differentiate Inclusion Conjunctivitis and Trachoma: • Inclusion conjunctivitis occurs in SEXUALLY ACTIVE adolescents or adults, whereas active, follicular trachoma usually occurs in young children or others living in or exposed to a community with endemic trachoma. • Conjunctival scarring is VERY RARE in adult inclusion conjunctivitis. • HERBERT’S PITS are a hallmark of trachoma. Adult and neonatal inclusion conjunctivitis Treatment: Adult • Azithromycin, 1 g in a single dose • Doxycycline, 100 mg orally twice daily for 7 days • Erythromycin, 2 g/d for 7 days. (for tetracycline resistant or pregnant woman) • Treat sexual partner. Newborn • Oral erythromycin suspension, 50 mg/kg/d in four divided doses for at least 14 days • Why Systemic not Topical? • Chlamydial infection also involves the respiratory and gastrointestinal tracts.