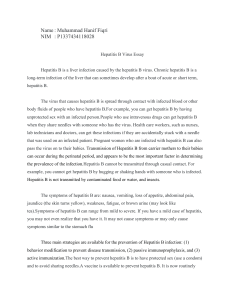
Clinical Practice Guidelines EASL Clinical Practical Guidelines on the management of acute (fulminant) liver failureq European Association for the Study of the Liver ⇑ Summary The term acute liver failure (ALF) is frequently applied as a generic expression to describe patients presenting with or developing an acute episode of liver dysfunction. In the context of hepatological practice, however, ALF refers to a highly specific and rare syndrome, characterised by an acute abnormality of liver blood tests in an individual without underlying chronic liver disease. The disease process is associated with development of a coagulopathy of liver aetiology, and clinically apparent altered level of consciousness due to hepatic encephalopathy. Several important measures are immediately necessary when the patient presents for medical attention. These, as well as additional clinical procedures will be the subject of these clinical practice guidelines. Ó 2016 European Association for the Study of the Liver. Published by Elsevier B.V. All rights reserved. Introduction The term acute liver failure (ALF) is frequently applied as a generic expression to describe patients presenting with or developing an acute episode of liver dysfunction. It is characterised by a deterioration in liver function tests, and potentially associated with dysfunction in other organs. ALF is frequently, but often incorrectly used to describe both acute deterioration in liver function in patients with chronic liver disease (a condition that should be termed acute-on-chronic liver failure [AoCLF]), or liver involvement in systemic disease processes. Liver injury secondary to alcohol, which presents as alcoholic hepatitis, and other forms of AoCLF, can be difficult to distinguish from ALF on occasion. However, there are clear differences, and different forms of management are required. Following extensive liver resection, patients with or without underlying chronic liver disease, may develop a clinical Received 7 December 2016; accepted 7 December 2016 q Clinical practice guidelines panel: Chair: Julia Wendon; Panel members: Juan Cordobay, Anil Dhawan, Fin Stolze Larsen, Michael Manns, Frederik Nevens, Didier Samuel, Kenneth J. Simpson, Ilan Yaron; EASL Governing Board representative: Mauro Bernardi ⇑ Corresponding author. Address: European Association for the Study of the Liver (EASL), The EASL Building – The Home of European Hepatology, 7 Rue Daubin, 1203 Geneva, Switzerland. Tel.: +41 (0) 22 807 03 60; fax: +41 (0) 22 328 07 24. y Juan Cordoba passed away during the preparation of this chapter. syndrome of jaundice, coagulopathy and hepatic encephalopathy (HE). The presentation is very similar to that of a posttransplant ‘‘small for size syndrome” scenario. These syndromes are not considered within the scope of ALF, but do feature in some ALF databases, such as the European Liver Transplant Registry (ELTR). Extensive liver trauma is also included in ALF databases, but is not a cause of ALF unless there is loss of both venous and arterial inflows. In the context of hepatological practice, ALF refers to a highly specific and rare syndrome, characterised by an acute abnormality of liver blood tests in an individual without underlying chronic liver disease. The disease process is associated with development of a coagulopathy of liver aetiology, as opposed to the coagulation disturbance seen in sepsis, and clinically apparent altered level of consciousness due to HE. The condition of patients who develop coagulopathy, but do not have any alteration to their level of consciousness is defined as acute liver injury (ALI). Thus, the term ALF is appropriately used to describe patients who develop both coagulopathy and altered mentation and will be the subject of these clinical practice guidelines. The features of coagulopathy, increased serum transaminases, abnormal bilirubin and altered levels of consciousness may be seen in patients with a variety of systemic disease processes. Therefore, if there is no primary liver insult, these patients should be considered to have a secondary liver injury and not ALF; management should focus on the treatment of any underlying disease processes. The evidence and recommendations in these guidelines have been graded according to the Grading of Recommendations Assessment Development and Evaluation (GRADE) system [1]. The strength of recommendations reflects the quality of the underlying evidence. The GRADE system offers two grades of recommendation: strong (1) or weak (2) (Table 1). The CPGs thus consider the quality of evidence: the higher the quality of evidence, the more likely a strong recommendation is warranted; the greater the uncertainty, the more likely a weaker recommendation is warranted. Definitions and main clinical features of ALF The clinical course of ALF is initiated with a severe ALI. This is characterised by a two- to threetimes elevation of transaminases (as a marker of liver damage) associated with impaired liver function, i.e., jaundice and coagulopathy, in a patient without a Journal of Hepatology 2017 vol. 66 j 1047–1081 Clinical Practice Guidelines chronic liver disease. This clinical description originated from observations of drug related hepatotoxicity, but is applicable to all presentations [2]. ALF was originally defined by Trey and Davidson in 1970 as fulminant liver failure, which was ‘‘a potentially reversible condition, the consequence of severe liver injury, with an onset of encephalopathy within 8 weeks of the appearance of the first symptoms and in the absence of pre-existing liver disease” [3]. In 1993, the syndrome was redefined to take into account the aetiology, frequency of complications and prognosis (Table 2) [4]. Considering jaundice as the first symptom, hyperacute liver failure describes patients developing HE within 7 days of noting jaundice. Acute liver failure occurs when patients develop HE between 8 and 28 days of noting jaundice; and subacute liver failure describes HE occurring within 5–12 weeks of jaundice (Fig. 1). Disease duration of greater than 28 weeks before the onset of encephalopathy is categorised as chronic liver disease. The International Association for the Study of the Liver (IASL) sub-committee statement (1999) defined hyperacute ALF as less than 10 days, fulminant ALF as 10 days to 30 days and subacute hepatic failure as 5 to 24 weeks [7]. Hyperacute presentations consist of severe coagulopathy, markedly increased serum transaminases and initially only moderate, if any, increase in bilirubin [8]. In contrast, subacute/subfulminant presentations often have a milder increase in serum transaminases, deep jaundice and mild to moderate coagulopathy [5,9]. It should be noted, however, that serum transaminase levels may not be considered a fully reliable parameter for diagnosis. Patients with subacute ALF often also have splenomegaly, ascites, and a shrinking liver volume. Once HE develops, these patients have a very low chance of spontaneous survival. In contrast, hyperacute presentations have a much greater chance of spontaneous recovery, despite having significant extrahepatic organ failure [10]. The disturbances to coagulation required to define ALF are determined by a prolongation of International Normalised Ratio (INR), usually >1.5, or a prolongation of prothrombin time (PT) [11]. Although this remains, at present, the accepted definition, it could be argued that a greater prolongation of INR should be required to define ALF. However, the Table 1. Grading evidence and recommendations (adapted from GRADE system). Grade I II-1 II-2 II-3 III Grade 1 2 1048 of evidence Randomized, controlled trials Controlled trials without randomization Cohort or case-control analytical studies Multiple time series, dramatic uncontrolled experiments Opinion of respected authorities, descriptive epidemiology of recommendation Strong recommendation: Factors influencing the strength of the recommendation included the quality of the evidence, presumed patient-important outcomes, and cost Weaker recommendation: Variability in preferences and values, or more uncertainty: more likely a weak recommendation is warranted. Recommendation is made with less certainty: higher cost or resource consumption INR is not standardised, and was designed to monitor warfarin therapy [12]. As a more accurate marker many clinicians would now suggest prolongation of PT in the context of the normal range for a particular laboratory. The other defining features of ALF, i.e., jaundice and HE, are required to be clinically manifested. However, in very young children and neonates, ALF may occur in the absence of HE, albeit with a definition that requires a much greater degree of coagulopathy (INR >4) [10]. Initial mental alterations may be subtle and therefore should be actively sought. Efforts have been made to develop more sensitive measures to define early grades of HE, but they are not available in routine clinical settings and certainly not in district hospitals where most patients first present for medical attention [13]. The concept of minimal HE is well recognised in patients with cirrhosis, but is poorly characterised in patients with ALF. Characterisation of minimal HE may be a useful tool in clarifying management plans for those with subacute presentations, although less relevant to hyperacute and acute ALF presentations. In subacute liver failure, the presence of HE usually occurs late in the disease course and is often a manifestation of infection; once HE develops the patient has a very short window to obtain a liver transplant, if any. Recent proposals suggest that in an appropriate clinical context accompanied by a shrinking liver volume, super urgent listing could be undertaken in this cohort, without the presence of clinically clear encephalopathy. Even with a definition set there are clear differences between acute and hyperacute liver failure (which have similar phenotype and clinical course), and subacute liver failure (which presents with a different clinical course). Separation of these two groups should be considered in future guidance, regarding prognosis and clinical management pathways. Another prerequisite for defining cases of ALF is the absence of previous severe fibrotic or cirrhotic chronic liver disease. Specific exceptions are the acute de novo presentation of autoimmune hepatitis and Budd-Chiari syndrome. In these conditions, an underlying chronic disease will not have been recognised or diagnosed previously, and there should be no clinical or histological evidence of cirrhosis. Wilson disease is another exception category; a clinical scenario when there is a clear chronic liver disease with splenomegaly, albeit frequently undiagnosed. The precipitant event is often a viral infection, [14] or in adolescents, non-compliance with therapy. Nevertheless, these patients are considered as having ALF since they share the poor prognosis, a common clinical picture of acute failure of the liver, and present with significant coagulopathy and encephalopathy. A small group of patients whom frequently cause consternation are those without overt fibrosis but with evidence of a liver pathology (e.g., metabolic syndrome and fatty liver, hepatitis C or B), who then develop an ALI. These patients may progress to encephalopathy, severe coagulopathy, and elevated serum transaminases. In the context of a clinical scenario, supported by ultrasound and axial imaging of no overt fibrosis or portal hypertension these patients would normally be categorised as ALF. Journal of Hepatology 2017 vol. 66 j 1047–1081 JOURNAL OF HEPATOLOGY Table 2. The clinical course of different ALF aetiologies. Precipitant Examples Presentation Viral Drugs/toxins Hepatitis A, E, B (less frequent CMV, HSV, VZV, Dengue) Paracetamol (acetaminophen), phosphorous, Amanita phalloides Anti-tuberculous, chemotherapy, statins, NSAI, phenytoin, carbamazepine, ecstasy, flucloxacillin Budd Chiari Hypoxic hepatitis Pre-eclamptic liver rupture, HELLP, fatty liver of pregnancy Wilson disease, autoimmune, lymphoma, malignancy, HLH Acute/fulminant Acute/fulminant and subacute/subfulminant Acute/fulminant Vascular Pregnancy Other Acute/fulminant and subacute/subfulminant Acute/fulminant Acute/fulminant Acute/fulminant and subacute/subfulminant CMV, cytomegalovirus; HSV, Herpes simplex; NSAI, non-steroidal anti-inflammatory; HELLP, haemolysis, elevated liver enzymes, low platelets; HLH, haemophagocytic lymphohistiocytosis. Recommendations Severe acute liver injury defines a syndrome characterised by markers of liver damage (elevated serum transaminases) and impaired liver function (jaundice and INR >1.5) which usually precedes clinical encephalopathy (evidence level II-2, grade of recommendation 1). Patients with an acute presentation of chronic autoimmune hepatitis, Wilson disease and Budd-Chiari syndrome are considered as having ALF if they develop hepatic encephalopathy, despite the presence of a pre-existing liver disease in the context of appropriate abnormalities in liver blood tests and coagulation profile (evidence level II-2, grade of recommendation 1). The clinical appearance of hepatic encephalopathy is crucial for the diagnosis of ALF but mental alterations may be initially subtle and intensive screening at the first sign of hepatic encephalopathy is mandatory (evidence level II-2, grade of recommendation 1). Considerations for future studies Biomarkers to help predict the progression from ALI to ALF. Development and dissemination of better tests for subtle hepatic encephalopathy in patients with subacute presentations. Review of INR/prothrombin cut-off for definition of ALF in the context of both hyperacute, acute and subacute liver failure. Burden of ALF within Europe The burden of ALF within the European Union (EU) remains unclear, with no collection of data regarding prevalence or incidence. Estimates are based on data presented in clinical series from referral and transplant units. Analysis of liver transplantation (LTx) data in the ELTR demonstrates that only 8% of all transplants are performed because of ALF as the primary indication. Sub-analysis of this 8% shows that 19% of cases are related to viral infection, 18% to drug-induced liver injury, 4% secondary to toxic insults and 3% postoperative or traumatic events, whilst 56% are attributable to unknown or other causes [15]. LTx is utilised in a minor proportion of patients with ALF; only 18.2% of patients received LTx according to the Kings College ‘‘Look-Back” [8]. However, the utilisation of LTx varies between countries, within different transplant units in a single country and between different aetiologies (Table 3). The incidence of virally induced disease has declined substantially in Europe. However, worldwide (especially Asia and Africa), it remains the commonest cause of ALF, with hepatitis A, E and B being the predominant causative viruses. The most frequent aetiology of ALF in Europe is now drug-induced liver injury (DILI); in some areas, this is predominantly from paracetamol (acetaminophen) overdose (POD), whilst in others non-paracetamol-induced drug toxicity prevails [10,27,28]. Estimated incidence of ALF in Scotland, which has a single national centre for referral, was 0.62/105/year. POD was the single most common cause, with an incidence of 0.43/105/year. Adding further complexity in estimating the true burden of ALF within the EU is the report from the same region that suggests less than 50% of cases that die following POD are transferred to this national referral centre [29]. What is clear is that ALF is a rare clinical condition but the true incidence across the EU is unknown, and disease burden is not clearly defined. Recommendations ALF is a rare diagnosis and multicentre data, such as the European Acute Liver Failure Registry, is required to assess outcome, optimal management and conduct appropriate multicentre studies (evidence level II-2, grade of recommendation 1). Whilst hyperacute and acute syndromes are usually easily diagnosed, subacute ALF may be mistaken for cirrhosis and the opportunity to be considered for transplantation lost (evidence level II-2, grade of recommendation 1). Clinical utilisation of transplantation varies upon aetiology and region (evidence level II-3, grade of recommendation 2). Journal of Hepatology 2017 vol. 66 j 1047–1081 1049 Clinical Practice Guidelines Jaundice to encephalopathy interval (weeks) 0 1 2 4 8 12 // (a) O’Grady et al. [4] ‘Hyper acute’ ‘Acute’ ‘Sub acute’ (b) Bernuau et al. [5] ‘Fulminant’ ‘Sub fulminant’ (c) Japanese consensus [6] ‘Fulminant’ Sub-class: ‘Acute’ ‘Late-onset’ ‘Sub acute’ Fig. 1. A summary of sub-classifications of ALF. Recommendations Considerations for future studies Enrolment of all patients with ALF into a common webbased database with internationally agreed definitions of ALF and sub-classification. Internationally accepted assessment of coagulation abnormalities in ALF. Development of EU wide epidemiological studies to define ALF and ALI prevalence and incidence. Assessment and management at presentation Several important measures are immediately necessary when the patient presents for medical attention (Table 4). Early discussion with a tertiary liver centre should be undertaken, even if the patient is not yet considered for transfer. Rule out the presence of cirrhosis and/or alcoholic-induced liver injury The clinical picture and radiology of patients with ALF, especially in the case of subacute ALF, can mimic cirrhosis. The loss of hepatic mass and regenerative nodules induce irregular contours of the liver. This, along with the presence of ascites and mild splenomegaly, are often signs radiologists use to diagnose the presence of cirrhosis. Access to medical history is therefore crucial. Liver biopsy, preferably by the transjugular route, can be useful to exclude cirrhosis, malignancy or alcohol-induced ALI. Liver biopsy has also been undertaken by mini laparoscopy without bleeding risk, but the risk of general anaesthesia and encephalopathy must be considered [30]. Liver biopsy is not helpful, however, for a prognosis based on the degree of liver necrosis, due to the problem of sample error [31]. 1050 The clinical picture and the radiology of subacute liver failure can mimic cirrhosis (evidence level II-3, grade of recommendation 1). The indications for liver biopsy in ALF are limited, and should be performed preferably by a transjugular route, in a centre experienced in its use, and with access to a histopathologist with liver experience. Incidence of underlying chronic liver disease, malignancies or alcoholinduced liver disease should be excluded if possible, but this does not provide prognostic information (evidence level II-3, grade of recommendation 1). Early referral of patients to a specialist centre will allow appropriate delineation of those likely to benefit from transplantation and offers an environment where focused expertise provides the greatest chance of spontaneous survival without LTx (evidence level III, grade of recommendation 1). The search for an aetiology The aetiology of ALF is an important indicator for prognosis and the treatment strategy, especially in the necessity for emergency LTx (Table 5). Clinical features may be typical in certain causes of ALF (Table 6). Aetiologies with no indication for emergency LTx Malignant infiltration of the liver. Extensive malignant infiltration of the liver, which can occur in metastatic breast cancer and lymphoma, can result in ALI or ALF. It is important to make this diagnosis early, since these patients are not candidates for LTx. In patients with a history of cancer or hepatomegaly, malignant infiltration should be ruled out with imaging and/or liver biopsy. Liver imaging requires experienced review, frequently has a pattern of diffuse infiltration as opposed to multiple deposits, and can be difficult to define as a likely malignant infiltrative picture Journal of Hepatology 2017 vol. 66 j 1047–1081 JOURNAL OF HEPATOLOGY Table 3. Epidemiological studies of ALF in different countries. Country UK* US Canada Scandinavia France Spain Chiley Australasia Sudan India Germany Reference Bernal et al. [16] 310 1994– 2004 43 8 Ostapowicz et al. [17] 308 1998– 2001 39 13 Tessier et al. [18] 81 1991– 1999 15 12 Brandsaeter et al. [19] 315 1990– 2001 17 10 Ichai et al. [20] 363 1986– 2006 7 21 Escorsell et al. [21] 267 1992– 2000 2 14 Uribe et al. [22] 27 1995– 2003 0 7 Gow et al. [23] 80 1988– 2001 36 6 Mudawi et al. [24] 37 2003– 2004 0 8 Khuroo et al. [25] 180 1989– 1996 0 0.6 Hadem et al. [26] 109 2008– 2009 9 32 7 12 30 12 33 37 37 14 27 21 30 13 17 19 27 16 43 17 18 21 32 15 44 11 34 10 38 27 68 (44 Hep E) 31 0 No. of cases Years Paracetamol (%) Non-paracetamol drug reactions (%) Hepatotropic viruses (%) Indeterminate (%) Other causes (%) * y 24 14 Patients listed for orthotopic liver transplantation only. Paediatric patients only. outside a specialist centre. The liver biochemistry classically shows an elevated alkaline phosphatase and gamma-glutamyl transferase but on occasions may present with marked increase in serum transaminases, caused by hepatocyte ischaemia resultant upon the infiltration. In patients with lymphoma, a greater elevation of lactate dehydrogenase is observed compared to serum transaminases [32,33]. Consideration of an underlying malignant process and potential infiltration should also be considered in acute presentations of Budd-Chiari syndrome [34]. Acute ischaemic injury. Acute ischaemic injury of the liver is especially common in elderly patients. The risk of this condition is increased in patients with cardiovascular disorders and severe congestive heart disease. Ischaemic injury often occurs in the presence of right heart dysfunction and associated liver congestion, with a subsequent episode of hypoxia or hypotension (so called hypoxic hepatitis). However, the absence of a documented episode of hypotension or hypoxia does not exclude this condition. Hypoxic hepatitis has a prevalence of between 1.2 and 11% in intensive care series. Three aetiological subgroups may be distinguished by respiratory failure, cardiac failure and septic shock/hypotension [35]. Hypoxic hepatitis is a secondary form of ALF. Therefore, the primary presenting organ failure needs to be addressed and managed to facilitate liver recovery [36], and LTx should not normally be considered. A characteristic pattern of liver blood tests are seen, which are similar to those observed in N-nitrosodimethylamine (NDMA) and paracetamol overdose. Aspartate transaminase (AST) are often >10,000 IU/L and at least twice the value of alanine aminotransferase (ALT), and frequently, bilirubin levels are normal at initial presentation. Marked elevation of transaminases and severe coagulopathy are seen, as with other causes of hyperacute ALF such as paracetamol and ecstasy (3,4-Methylenedioxymethamphetamine [MDMA]) overdose [37–39]. HE and hyperammonaemia are also not infrequent. Liver ischaemia is also seen following trauma and surgical mishap when there is loss of vascular inflow into the liver. In these cases, LTx should be not considered unless there is loss of all vascular inflows. Other systemic diseases. Other conditions may also result in ALF but are not an indication for LTx. Haemophagocytic lymphohistiocytosis (HLH) may be precipitated by viral or fungal infections or occur in the context of haematological malignancy [40]. Similarly, infectious disease processes such as malaria, dengue and rickettsiosis may result in secondary liver failure [41]. ALF may also be seen in the context of systemic mitochondrial failure following some toxic ingestions (yellow phosphorous) or related to some drug related toxicities. The role of LTx in the latter setting is not clear. Recommendations In patients with a history of cancer or significant hepatomegaly, malignant infiltration should be excluded by imaging or liver biopsy (evidence level II-3, grade of recommendation 1). Acute ischaemic injury will resolve after improvement of haemodynamic status, and is not an indication for emergency LTx. It can occur in the absence of a proven period of hypotension (evidence level II-3, grade of recommendation 1). Table 4. Immediate measures at presentation of patients with ALF to medical care. In patients with severe ALI, screen intensively for any signs of hepatic encephalopathy. Exclude the presence of cirrhosis, alcohol induced liver injury or malignant infiltration of the liver. Consider whether the patient does not have contraindications for emergency LTx: the finding of contraindications should not preclude transfer to a tertiary unit. Searching for an aetiology allows treatment to be instituted and facilitates prognostic stratification. Transfer to a specialised unit early if the patient has an INR >1.5 and onset of hepatic encephalopathy or other poor prognostic features. Early discussion with a transplant unit even if the patient does not need transfer at that time point. Journal of Hepatology 2017 vol. 66 j 1047–1081 1051 Clinical Practice Guidelines Table 5. Primary or secondary causes of ALF and need for transplantation. Disease group Hepatic/primary ALF (Emergency transplantation may be a treatment option) Extrahepatic/secondary liver failure and AoCLF (Emergency transplantation is not a treatment option) Acute liver failure Drug related Acute viral hepatitis Toxin-induced ALF Budd-Chiari syndrome Autoimmune Pregnancy related Ischaemic hepatitis (HH) Systemic diseases: Haemophagocytic syndromes Metabolic disease Infiltrative disease Lymphoma Infections (e.g., malaria) Chronic liver disease presenting with a phenotype of ALF Fulminant presentation of Wilson disease Liver resection for either secondary deposits or primary liver cancer Alcoholic hepatitis Autoimmune liver disease Budd-Chiari HBV reactivation Aetiologies which form a possible indication for emergency LTx Drug-induced hepatotoxicity Paracetamol overdose. Paracetamol intoxication can be a single time point POD with intentional suicide or para-suicidal motivation, a situation especially seen in the UK. Alternatively, accidental hepatotoxicity can occur in patients taking excessive amounts of paracetamol to relieve pain, which is often associated with ingestion over several days (staggered presentation). Accidental POD can be associated with alcohol dependence, ingestion of multiple paracetamol containing compounds or the use of opioid-paracetamol compounds [8,42–44]. Increased sensitivity to paracetamol is seen in those with decreased glutathione reserves, e.g., fasting, excessive alcohol consumption and in those taking certain regular medications, such as phenytoin [45]. Toxicology screening and determination of the circulating paracetamol level needs to be done at admission in every patient, especially in cases with hyperacute ALF and significantly elevated serum transaminases. However, even though paracetamol metabolism is reduced with liver failure, paracetamol is usually undetectable at the time of presentation, and aetiology often has to be based on clinical presentation, history and typical laboratory results. POD-induced hepatotoxicity is characterised by extreme elevations of serum aminotransferase (usually >10,000 IU/L) and normal bilirubin levels. Metabolic acidosis, elevated serum lactate, hypoglycaemia and acute kidney injury (AKI) can occur in early stages of clinical evolution. Accidental staggered POD produces smaller elevations of serum aminotransferase, but more marked organ failure at presentation is frequently observed. This cohort is less easy to stratify regarding prognosis, as their INR or PT are less elevated. Other scoring systems, such as sequential organ failure assessment (SOFA) score, may be preferred [16,27,46]. Very early presentation of patients with significantly elevated paracetamol levels can be associated with marked metabolic acidosis and elevated lactate, but only mild elevation of transaminase levels and minimal, if any, coagulopathy. This is a separate entity to the later ALF that may develop. This clinical syndrome is considered as a direct drug effect, relating to functional mitochondrial standstill, and resolving with falling paracetamol levels. These patients should be treated with appropriate fluid resuscitation, N-acetylcysteine (NAC), and may need renal replacement therapy (RRT) to treat the acidosis. In these cases, other compounding aetiologies should also be sought such as salicylate, tricyclic or methanol ingestion. The clinical evolution of POD is often that of rapidly progressive multi-organ failure (MOF) and HE, which may progress from a mild grade 1 to grade 4 coma over a period of hours. Patients who do not meet criteria for emergency LTx have a good prognosis, and those who meet the criteria may still have a survival rate of 20–40% with modern intensive care management, according to recent reports. Significantly improved outcomes with medical management have been reported, and are achieved despite poor prognostic criteria [16,46]. The clinical presentation and evolution is different between hepatotoxicity induced by POD and most Table 6. Differential diagnosis of ALF based on clinical features. Aetiology Clinical features Malignant infiltration Acute ischemic injury History of cancer, massive hepatomegaly; elevated alkaline phosphatase or other tumour markers. Marked elevation of aminotransferases, increased lactic dehydrogenase and creatinine, which normalise soon after stabilisation of haemodynamic instability. Patients with severe congestive heart disease or respiratory disease. Very high levels of aminotransferases and low level of bilirubin. Rapidly progressive disease, acidosis and renal impairment. Low phosphate may be seen as a good prognostic marker but replacement is required. Subacute clinical course can mimic cirrhosis, clinically and radiographically. Paracetamol Non-paracetamol drug toxicity Acute Budd-Chiari syndrome Wilson disease Mushroom poisoning Autoimmune 1052 Abdominal pain, ascites and hepatomegaly; loss of hepatic venous signal and reverse flow in portal vein on ultrasound. Young patient with Coombs (DAT) negative haemolytic anaemia with a high bilirubin to alkaline phosphatase ratio; KayserFleischer ring; low serum uric acid level; markedly increased urinary copper. Severe gastro-intestinal symptoms after ingestion; development of early AKI. Usually subacute presentation – may have positive autoantibodies, elevated globulin and characteristic lymphocyte pattern when compared to viral and seronegative aetiologies. Journal of Hepatology 2017 vol. 66 j 1047–1081 JOURNAL OF HEPATOLOGY other drugs causing ALF. NAC is associated with improved outcome in patients presenting with POD [47–49]. Other drug toxicities are usually associated with a less significant elevation of serum aminotransferases, higher bilirubin levels and less associated extrahepatic organ dysfunction than are observed in patients with POD. Often a mixed or cholestatic pattern of liver function abnormalities are observed. The mode of cell death is different depending on aetiology, and different therapeutic interventions may be required to promote regeneration and repair [50–52]. Non-paracetamol. Less than 10% of patients with nonparacetamol DILI progress to ALF but if they do, up to 80% die or require emergency LTx [2]. Drug-induced ALF arises more often in older patients, especially above 60 years [53–56]. A hepatocellular DILI normally presents with an acute ALF clinical course, compared with cholestatic DILI, which is more likely to lead to a subacute course. A hypersensitivity reaction is uncommon and seen in less than one third of patients [57–59]. In contrast with most DILI, ecstasy-induced liver injury is a hyperacute presentation resulting from or associated with severe hyperthermia with multiple organ involvement, profound coagulopathy and severe rhabdomyolysis. This clinical picture is identical to other forms of heat shock related liver injury [37,38]. Assessment of prognosis in the first few day can prove more challenging in multi-organ compared to primary hepatic failure. LTx is rarely (if ever) required, despite profound abnormalities in blood tests and physiology. In the majority of cases LTx will not alter the outcome. Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome is a very rare presentation and should always be considered in those with fever, eosinophilia, marked cutaneous rash and lymphadenopathy. Sulphur containing compounds, some anticonvulsants and antimicrobials are more often associated with DRESS. High dose steroid therapy should be considered prior to the development of ALF in patients with DRESS [60]. Concurrent viral infections should always be sought in those with DILI, as they are frequent and have been associated as trigger factors for DILI. The classes of drugs most frequently associated with ALF are antituberculosis drugs (especially isoniazid [61]), antibiotics (especially nitrofurantoin and ketoconazole), anti-epileptics (especially phenytoin and valproate), non-steroidal antiinflammatory drugs, and a wide group of other medication such as propylthiouracil and disulfiram [56,62]. Guidelines have been issued by various thoracic societies for the management and withdrawal of anti-tuberculous chemotherapy in patients who develop hypertransaminasaemia or jaundice [63]. Some patients will not automatically report the ingestion of drugs, especially in the context of illicit drugs, herbal medicine products or nutritional supplements. The latter is especially prevalent in East Asia [62]. Intensive questioning of the patient and their relatives is necessary at different opportunities and by several physicians to comprehensively exclude a drug cause for ALF. DILI may only become symptomatic several weeks after ingestion. A record of all drugs (prescribed and non-prescribed), vitamin supplements and herbal medicines taken within the last 6 months should be collected. Other causes of severe ALI should always be ruled out, since DILI is often a diagnosis of exclusion. This especially applies to autochthonous hepatitis E virus (HEV) infection, which may be misdiagnosed as DILI and occurs more frequently in similar demographic groups. In rare cases, drugs such as long-acting niacin, cocaine or methamphetamine, can induce liver ischaemia via hypoperfusion. Acute ischaemic injury caused by these agents is characterised by a marked elevation of both aminotransferases and lactic dehydrogenase, a rapidly progressive prolongation of the PT, and increased serum creatinine. These abnormalities normalise soon after hemodynamic stabilisation [64]. As with all aetiologies of hypoxic hepatitis, the majority of cases survive with medical management alone. Viral hepatitis. The following hepatic viruses can cause ALF: hepatitis B virus (HBV), hepatitis A virus (HAV) and HEV. HBV. HBV is the most common viral cause of severe ALI and ALF, due to either de novo infection, delta superinfection or reactivation in a patient with previous HBV infection [65,66]. Vaccination has led to a significant drop in the incidence of HBV cases, with a concomitant fall in HBV induced ALF [67,68]. Fewer than 4% of cases with acute hepatitis B will develop ALF, but mortality is higher than in HAV or HEV infections [25,68–70]. Early treatment with antiviral therapy decreases the risk of progression to ALF [71]. Reactivation in chronic carriers occurs during or after treatment-induced immunosuppression for solid organ or haematological malignant disease and has a higher mortality than de novo infections [72,73]. Increasingly, reactivation may be seen in those patients treated with rituximab, either in the context of chemotherapy or treatment of immune mediated diseases [74,75]. Screening of populations is essential prior to significant immunosuppression or administration of antiviral prophylactic treatment in patients with previous HBV exposure. HBV related ALF presents with an acute phenotype. As observed with other hepatitis viruses and causes of ALF, the prognosis of HBV-induced ALF is worse in the elderly and in those with severe co-morbidities [76]. HAV. Less than 1% of patients with acute HAV will develop ALF, and several cofactors will affect its evolution [77]. Usually, hepatitis A has a hyperacute or acute clinical course. ALF due to HAV is also more common in older patients, and in this patient group has a worse prognosis [78,79]. HEV. Acute hepatitis due to HEV is most frequently seen in patients who recently travelled to endemic areas. However, sporadic cases of acute HEV are detected in Europe [80,81]. Hepatitis E results in a hyperacute pattern of ALF and although mortality is low, worse outcomes are observed in elderly patients, those with pre-existing but undiagnosed chronic liver disease and pregnant women [82–84]. The disease presentation in Asia and Africa is more severe than that seen in Europe [85]. Other viral infection. Herpes simplex virus types 1 and 2 and varicella zoster are other rare viral causes of ALF. Even though these infections are more commonly seen in immunosuppressed patients, they may also occur in immunocompetent individuals. The absence of skin lesions does not exclude the diagnosis. Screening of blood for cytomegalovirus (CMV) and Epstein–Barr virus (EBV) using nucleic acid testing should be undertaken in all patients where the aetiology of ALF is not clear [86,87]. The development of DILI can also be potentiated by the activation of the herpes and CMV viruses, along with host drug interactions [88]. The presence of these viral infections may not always represent the aetiology of the ALF but may be a co-factor and consideration for treatment. In the context of immunosuppression, such viral infections may also be of importance as a primary aetiology. Autoimmune hepatitis. The presence of other autoimmune disorders in a patient presenting with ALF should raise suspicion of autoimmune hepatitis as the aetiology. These patients often have an elevated globulin fraction and positive autoantibodies, but Journal of Hepatology 2017 vol. 66 j 1047–1081 1053 Clinical Practice Guidelines these may also be absent in a proportion of cases [89–92]. Equally however, mildly positive autoantibodies may be seen in a variety of aetiologies, and it should not be assumed that autoimmune disease is the primary driver of the liver injury. Liver biopsy may be required to determine the diagnosis. Treatment with steroids may be effective if given early. In the context of ALF, however, steroids are often ineffective and potentially deleterious, as they may favour septic complications [93]. Thus, a lack of improvement within seven days should lead to listing for emergency liver transplant (LT) without delay. Indeterminate aetiology. In some patients, usually presenting with an acute or subacute ALF phenotype, no aetiology can be identified [10]. A proportion of these patients may have taken drugs or xenobiotics, which they do not not (or cannot) recall. Others provide a history compatible with a viral phenotype, although no specific viral aetiological agent can be identified [89]. Some subsequently present with immune mediated features, suggesting that the original disease may have had an autoimmune aetiology. In some of these groups, as well as in those of a known aetiology, the potential for paracetamol induced co-toxicity may be raised by the presence of paracetamol adducts [42,94]. Equally, studies have suggested that some cases of presumed seronegative aetiologies may have a hepatitis E infection, and appropriate tests regarding sensitivity and specificity should always be undertaken [70]. Considerations for future studies Further continuous update of the European Acute Liver Failure Registry. Review of criteria defining poor prognosis in the context of modern critical care and support. Application of biomarkers to further delineate cofactors in the development of ALF (e.g., paracetamol adducts, viral nucleic acid testing). More uncommon aetiologies of ALF. In this group of aetiologies, a specific treatment or intervention can be started. However, in the majority of the cases, the positive effect of the treatment will often be too late to be beneficial. Therefore, if these patients fulfil criteria for LTx, consideration for emergency surgery should not be delayed. Budd-Chiari syndrome. An acute Budd-Chiari syndrome is characterised by abdominal pain, ascites and hepatomegaly. Diagnosis is made based on imaging of the liver. Testing for hypercoagulable conditions and screening for underlying malignancies are necessary [34,95]. Recommendations Drug-induced liver injury, especially paracetamol toxicity, is the most frequent cause of severe ALI and ALF. At admission, a toxicology screen and determination of paracetamol level are necessary in every patient, although levels will frequently be negative. If the patient already has coagulopathy and increased serum transaminases, N-acetyl cysteine therapy should be given (evidence level II-2, grade of recommendation 1). Prognosis is worse in patients with staggered ingestion of paracetamol. These cases are more likely to develop multiple organ failure when compared to those with single ingestion point (evidence level II-3, grade of recommendation 1). ALF caused by non-paracetamol drug-induced hepatotoxicity, is a diagnosis of exclusion (evidence level III, grade of recommendation 2). Screening for viral aetiologies and co-factor effects should always be undertaken (evidence level II-2, grade of recommendation 1). Autoimmune aetiology should be suspected in patients presenting other autoimmune disorders, elevated globulin fraction and autoantibodies. These features, however, may be absent and liver biopsy may be required. Early treatment with steroids may be effective; however, lack of an improvement within seven days should lead to listing for emergency LTx without any delay, as steroids may increase mortality because of septic complications (evidence level II-2, grade of recommendation 1). 1054 Wilson disease. The classic presentation of acute Wilson disease includes HE in young patients (<20 years) with a Coombs negative haemolytic anaemia, and high bilirubin to alkaline phosphatase ratio. In 50% of cases, Kayser-Fleischer rings are present. There is often renal dysfunction and serum uric acid level is low. Serum caeruloplasmin can be very low but may be normal or increased in the acute situation [96,97]. Serum caeruloplasmin is also reduced in 50% of other aetiologies of ALF. Serum and urinary copper are markedly increased [98,99]. There may be a concurrent viral precipitant or non-compliance with medication in a previously diagnosed case of Wilson disease. Prognosis is welldefined with specific prognostic modelling [100]. Mushroom poisoning. Mushroom poisoning, usually by amanita phalloides (the most toxic of the mushroom species regarding hepatotoxicity), can cause ALF [101,102]. Although it occurs very rarely, recent mushroom ingestion should always be sought in a patient with ALI or ALF. There is no routine laboratory test to identify the toxins. Severe gastrointestinal symptoms with profuse vomiting and diarrhoea within hours or a day after ingestion is suggestive for mushroom poisoning. The development of acute renal failure, secondary to volume depletion, normally precedes the development of liver failure. Prognosis should be judged in a similar way to the models for other hyperacute syndromes, such as paracetamol. Pregnancy related ALF. There are two hepatic emergencies which occur in the third trimester of pregnancy: haemolysis, elevated liver enzymes and low platelets (HELLP) syndrome and acute fatty liver of pregnancy (AFLP). HELLP should be differentiated from atypical haemolytic uraemic syndrome and thrombotic thrombocytopenic purpura [103]. AFLP is characterised by extensive hepatic steatosis and usually presents with abdominal pain and malaise. Transaminases are relatively low. Hypoglycaemia Journal of Hepatology 2017 vol. 66 j 1047–1081 JOURNAL OF HEPATOLOGY is common, and elevated urate levels are also seen as maybe polyuria and polydipsia. Other organ failures occur, including pancreatitis [87,103,104]. Maternal mortality is around 20%. Prompt delivery of the baby in both these emergency scenarios offers a good outcome, and emergency LTx is rarely needed. Persistent elevation of lactate levels in the presence of severe HE potentially best identifies patients at greatest risk of death or LTx. When liver failure occurs specifically in pregnancy, consideration should also be given to liver rupture associated with preeclampsia. This normally presents as sudden onset of right upper quadrant pain and requires distinction from pulmonary embolus. Management is normally conservative but may require laparotomy and packing if rupture through the capsule causes significant bleeding. Extensive subcapsular haematoma may result in ischaemic compression of liver parenchyma and rarely compression of the hepatic veins, resulting in a syndrome similar to Budd-Chiari [105]. ALF induced by hemi-hepatectomy. Extensive loss of liver parenchyma after resection of the liver can provoke ALI. Most patients will recovery spontaneously if resection is performed in the absence of an advanced liver disease. It is not an accepted indication for emergency LTx. However, emergency LTx has been reported in cases of ALF induced by living donor liver graft failure [106]. Hyperthermic injury from heat shock. This may be seen in association with recreational drug use, such as ecstasy, but may also be seen in those undertaking physical exertion in high ambient temperatures and following prolonged fitting, again usually in high ambient temperatures [107]. Secondary aetiologies of ALF/ALI. In any patient presenting with increased serum transaminases and/or cholestasis and coagulopathy, where the aetiology is not primarily hepatic in aetiology, screening for other factors should be undertaken. This should include sepsis [108], malaria, leptospirosis, rickettsial diseases, thyroid disease [40,109], Stills disease, and haemophagocytic syndromes [39,110]. The latter two lead to markedly elevated ferritin levels and elevated triglyceride levels in the latter. In Asia and Africa, ALF may be seen in conjunction with systemic multiple organ involvement following yellow phosphorous poisoning, a syndrome resulting in mitochondrial toxicity. These conditions are not commonly accepted indications for emergency LTx. Recommendations Assessment of the clinical context is crucial to identify less common causes of ALF (evidence level III, grade of recommendation 1). ALF presenting with gross ascites should lead to suspicion of acute Budd-Chiari syndrome. Diagnosis of this condition is based on imaging techniques (evidence level II-3, grade of recommendation 1). Coombs negative haemolytic anaemia and high bilirubin to alkaline phosphatase ratio are features of ALF due to Wilson disease (evidence level II-3, grade of recommendation 1). In cases of HELLP and AFLP, the treatment of choice is prompt delivery of the baby, especially in case of elevated lactate levels and hepatic encephalopathy. Screening for putative fatty acid defects should be offered (evidence level II-3, grade of recommendation 1). Screening for systemic diseases presenting as ALF should be undertaken (evidence level III, grade of recommendation 1). General support management outside ICU Clinical assessment A comprehensive clinical assessment and history taking of patients and their relatives at admission is of upmost importance with specific questions for aetiology, comorbid conditions, to exclude conditions which form no indication for emergency LTx. This should also help to define the interval between jaundice and the first signs of HE to classify the subtype of ALF (Table 7). Table 7. Anamnesis of patient and relatives at admission. Search for an aetiology: Use of medication (ask specifically for paracetamol and paracetamol containing compounds), herbal medicine and food supplements <6 month Pregnancy History of a chronic liver disease Substance abuse History of suicidal attempt/depression Gastrointestinal complaints after mushroom ingestion Conditions permissive for ALF: Travelling in viral hepatitis endemic areas (HBV, HEV) In receipt of immunosuppressive or chemotherapy History of autoimmune disease Conditions that may impact upon decision in respect to emergency LTx: Active and dependent alcohol or substance misuse (individualised decision making) History of cancer in recent past (specialist input required) Severe congestive heart disease or respiratory co-morbidity Interval between onset of jaundice and first signs of hepatic encephalopathy Journal of Hepatology 2017 vol. 66 j 1047–1081 1055 Clinical Practice Guidelines Table 8. Laboratory analyses at admission. For assessing the severity of the disease: PT, INR or factor V and full coagulation screen including fibrinogen Liver blood tests including LDH and conjugated and unconjugated bilirubin and creatinine kinase Assessment of renal function: urine output: hourly. low urea is a marker of severe liver dysfunction. creatinine may be difficult to assay in the context of elevated bilirubin. Arterial blood gas and lactate Arterial ammonia For aetiology: Toxicology screen in urine and paracetamol serum level Serological screen for virus infections HBsAg, anti-HBc IgM (HBV DNA), delta if positive for HBV anti HAV IgM anti-HEV IgM anti-HSV IgM, anti VZV IgM, CMV, HSV, EBV, parvovirus and VZV PCR Autoimmune markers: ANA, ASMA, anti-soluble liver antigen, globulin profile, ANCA, HLA typing For testing for complications: Lipase or amylase Laboratory investigation At admission, specific laboratory analyses are needed to assess the severity of the liver injury, to diagnose the aetiology, to define prognosis for patients who are candidates for emergency LTx, and to rule out complications such as acute pancreatitis (Table 8). Arterial blood gas may be considered alongside a baseline arterial ammonia measurement. Blood urea will frequently be pathologically low and is not a reflection of renal function, which is best assessed by urine output and creatinine. Diagnostic procedures, monitoring and standard care at admission Chest radiography, baseline echocardiography (ECG), and liver echography (interrogating patency and direction of flow in vessels in addition to liver texture and size, splenic size) should be obtained. Axial computed tomography (CT) imaging should be considered to examine liver texture and volume, vascular integrity, exclude pancreatitis and presence of umbilical vein patency (cirrhosis) (Table 9). At present, the most frequent causes of death in patients with ALF are MOF and severe sepsis. Therefore, the general supportive management of patients with ALF should focus on the prevention and prompt treatment of infections. Careful monitoring of organ function and appropriate management of dysfunction as early as possible should be carried out, as described in subsequent sections on specific organ support. The progression risk of HE must be recognised and emphasised, and appropriate nursing observations undertaken. The development of cerebral irritation or change in level of consciousness should be assumed to be HE. However, other causes should be sought and excluded, such as alcohol withdrawal or other metabolic causes. There is no evidence for the use of lactulose or rifaximin in the setting of ALF. Monitoring for neurological signs of worsening HE should be instituted at 2-hourly intervals. Development of HE grade 2 or more should result in transfer to a critical care area, with the skill to provide airway and ventilator management should the HE deepen. The use of sedative agents in a ward setting is contraindicated; all such patients should be transferred to a critical care environment. Although prolongation of clotting tests is a cardinal feature of ALF, bleeding is uncommon unless the platelet count is very low, combined with low fibrinogen, prolongation of activated partial thromboplastin time (APTT), factor V and INR [111]. Recent characterisation of the balanced disturbance of both pro- and anticoagulant factors occurring in patients with ALF, suggests Table 9. Diagnostic procedures, monitoring and standard care at admission. Diagnostic tests: Cultures (respiratory, blood, urine) Chest X-ray/ECG/liver echography: axial imaging of the abdomen and chest may also be required Cardiac ECG Routine monitoring: Oxygen saturation, blood pressure, heart rate respiratory rate, hourly urine output Clinical neurological status Standard care: Glucose infusions (10–20%): glycemic target ± 140 mg/dl, Na 135–145 mmol/L Stress ulcer prophylaxis Restrict clotting factors unless active bleeding N-acetylcysteine in early stage, even in non-paracetamol cases Preventative measures: Avoid sedatives Avoid hepatotoxic and nephrotoxic drugs In case of hepatic encephalopathy: 1056 Transfer to an appropriate level of care (ideally critical care) at the first symptoms of mental alterations Quiet surrounding, head of bed >30°, head in neutral position and intubate, ventilate and sedate if progresses to >3 coma. Low threshold for empirical start of antibiotics if hemodynamic deterioration and/or increasing encephalopathy with inflammatory phenotype In case of evolving HE intubation and sedation prior to the transfer Ensure volume replete and normalize biochemical variables (Na, Mg, PO4, K) Journal of Hepatology 2017 vol. 66 j 1047–1081 JOURNAL OF HEPATOLOGY that such patients have frequent procoagulant imbalances [112,113]. Prophylactic administration of coagulation factors is not advised because it will influence the INR or PT, the most important factors of prognosis, and is rarely if ever, clinically indicated. Patients with ALF are at risk of hypovolaemia due to poor oral intake, vomiting and vasodilation with an effective decrease in central blood volume. Fluid bolus therapy and then maintenance fluids may frequently be required but it is essential to maintain serum sodium in the normal range and avoid excessive fluid overload. Assessment of volume status in a ward environment may be challenging. In the initial phases of hyperacute and acute presentation, falls in lactate may allow assessment of volume responsiveness [114]. However, subsequent lactate reflects a composite measure of both increased production (peripheral aerobic glycolysis and decreased clearance due to hepatic metabolic capacity) [115]. Oral intake is encouraged if the patient is not too nauseated, but if HE progresses this should be avoided as patients may require urgent intubation. Insertion of nasogastric tubes prior to intubation is normally avoided due to risk of vomiting, aspiration, and inducing nasal trauma and associated bleeding. Stress ulcer prophylaxis is usually recommended [116,117], although there is no substantive data to support its use. NAC has not only been shown to decrease progression to liver injury if given early following POD (<15 h) [118], but also to have a beneficial effect on organ dysfunction when given up to 48 h following POD [49]. The beneficial effects of NAC may be mediated by its putative anti-oxidant attributes, delivery of a sodium load, anti-inflammatory mechanisms via nuclear factor kappa B (NFjB), or its vasodilatory effects improving microcirculatory flow [47,119,120]. In non-paracetamol ALF NAC did not improve survival overall, but did improve outcome in adults with mild grades of HE [121]. NAC was not shown to be beneficial in a recent paediatric study, albeit containing significant numbers of patients whose ALF was of metabolic cause, nor did it show benefit in a subsequent meta-analysis [122,123]. Animal data suggests that prolonged use of NAC may limit liver regeneration [124] but there are also studies suggesting it is beneficial promoting regeneration [125]. In addition, it is advisable to limit the clinical use of NAC to a maximum of 5 days duration, given its anti-inflammatory effects. After this time, functional immune-paresis becomes increasingly relevant when compared to the initial ALF associated cytokine storm and further functional immunosuppression is unlikely to benefit the patient and may increase risk of nosocomial sepsis [126,127]. Transfer to a specialised unit The evolution of ALF is highly unpredictable, especially hyperacute clinical presentations. All patients with a significant ALI should be considered for transfer to a LTx or tertiary care unit (Table 10). Even in those who are unlikely to be candidates for LTx should be considered for transfer to offer improved chances of survival. ALF is a rare clinical syndrome and the experience of specialised liver units is required to continually improve the outcome of these patients. Mental alterations may be subtle. Even mild HE can indicate a life-threatening situation within a few hours. Therefore, it is advised to consider transfer at the onset of any mental changes, if the INR is increased >1.5, or if there is hypoglycemia or metabolic acidosis. Prior to transfer, patient review should be obtained from senior colleagues in critical care with experience in the transfer of critically ill patients. In the scenario of an evolving HE, there is an indication for intubation and sedation to ensure a controlled and safe transfer. Transfer standards should be compliant with those of critical care societies [128]; appropriate fluids should be available for ongoing volume resuscitation, the patient maintained normoglycaemic, and vasopressors should be drawn-up and available. Pupils should be inspected and mannitol carried in case of the development of fixed dilated pupils in transit. Detailed guidance and discussion between the transferring and receiving team is essential, along with the clinical expertise to deal with acute deteriorations in a clinical condition. The insertion of central venous lines and arterial lines may be complicated by concerns regarding coagulopathy. Fresh frozen plasma, cryoprecipitate or factor concentrates should be avoided as they distort clinical decision making with respect to prognosis. Data now suggests that largely balanced coagulation disturbances without a bout of bleeding, in conjunction with isolated prolongation of INR, as well as very low platelets and fibrinogen, may be associated with an increased risk of bleeding. If the platelet count is low (<30,000/ll) platelets may be given before line insertion. If dynamic assessment of coagulation (thrombo-elastography) is available, this may provide reassurance [111,129]. Initially, patients may be managed with a radial arterial line and large bore peripheral cannulae. If there may be a need for vasopressors and the clinicians are concerned with the risk of an internal jugular line, then a femoral venous line may be inserted. This allows ease of access, direct pressure for bleeding and decreased risk of other organ damage if bleeding occurs. Line insertions should be undertaken by experienced individuals, ideally with ultrasound guidance ensuring the site of venous puncture is well below the inguinal ligament. Subclavian access should be avoided due to risk of complications. Recommendations Diagnosis of ALF should be always considered with respect to the full clinical picture; appropriate investigations and discussion with a tertiary centre should be undertaken. This is especially important in cases of subacute clinical course (evidence level III, grade of recommendation 1). Frequent senior clinical review (twice daily minimum) and assessment of physiological parameters, blood results and metabolic status should be carried out (evidence level III, grade of recommendation 1). Hourly urine output should be assessed as a marker of renal function, alongside creatinine (evidence level III, grade of recommendation 1). Clinical deterioration with extrahepatic organ involvement should result in transfer to critical care and tertiary centre (evidence level III, grade of recommendation 1). Journal of Hepatology 2017 vol. 66 j 1047–1081 1057 Clinical Practice Guidelines Table 10. Suggested criteria for referral of cases of ALF to specialist units. Paracetamol and hyperacute aetiologies Non-paracetamol Arterial pH <7.30 or HCO3 <18 INR >3.0 day 2 or >4.0 thereafter Oliguria and/or elevated creatinine Altered level of consciousness Hypoglycaemia Elevated lactate unresponsive to fluid resuscitation pH <7.30 or HCO3 <18 INR >1.8 Oliguria/renal failure or Na <130 mmol/L Encephalopathy, hypoglycaemia or metabolic acidosis Bilirubin >300 lmol/L (17.6 mg/dl) Shrinking liver size Coagulation/hemostasis Neurological = Cerebral oedema Unbalanced hemostasis Thrombocytopenia Infection Cranial hypertension Brain death Acute liver failure Bacterial, fungal Pneumopathy Septicemia Urinary infection Metabolic Hypoglycemia Hyponatremia Hypophosphoremia Hypokalemia Haemodynamic Pulmonary Renal Hyperkinetic syndrome Arrhythmia Pneumopathy Acute respiratory distress syndrome Pulmonary overload Toxic Functional Fig. 2. Main organ specific complications in ALF. Considerations for future studies Biomarkers to help predict deterioration and likely progression of disease. Assessment of volume status and appropriate fluids in a ward setting. Point of care assessment for sepsis. Organ specific management (Fig. 2) Cardiovascular management Most patients presenting with ALF or severe ALI develop systemic vasodilation with reduced effective central blood volume. Early presentation with hyperlactataemia is probably a consequence of volume depletion, and responds to appropriate volume loading. Thereafter, ongoing hyperlactataemia is likely to reflect the severity of the underlying liver failure; the liver in unable to metabolise the increased lactate production seen in response to sympathetic drive and accelerated aerobic glycolysis (Fig. 2) [130–133]. 1058 In addition to hyperlactataemia, if clinical examination at initial presentation reveals no evidence of cardiorespiratory disease (e.g., jugular venous pressure not elevated), and the patient has evidence of end organ dysfunction (peripheral hypoperfusion, acidosis, oliguria or renal failure,) then it is highly likely that they are volume depleted and will respond to an appropriate fluid challenge. There is little evidence supporting the use of any specific fluid for volume loading in ALF. However, general critical care literature supports the use of crystalloid fluid over colloid [130–133]. The choice should be guided by biochemical parameters and clinical status; initially normal saline may be effective. Hyperchloraemia should be avoided, as it has been associated with increased risk of renal failure and other morbidities [134,135]. Further crystalloid loading may then be undertaken with Ringers lactate (recognising the risk of hypotonicity) or a balanced solution as required. Balanced solutions are buffered with either bicarbonate or acetate. Although most patients with cirrhosis can metabolise acetate, those with severe hyperacute and acute presentations of ALF may have a risk of a decreased metabolic capacity in this clinical context. The role of albumin has not been investigated in ALF. Subgroup post hoc analysis in the Saline vs. Albumin Fluid Evaluation (SAFE) study suggested a benefit in severe sepsis and septic shock, but detrimental in patients with traumatic brain injury [136,137]. Patients with ALF could be considered to phenotypically represent both groups; a similar trend was reported in the more recent Albios study Journal of Hepatology 2017 vol. 66 j 1047–1081 JOURNAL OF HEPATOLOGY where possible improved outcome in septic shock was seen [138]. If used in this context, albumin should be viewed more as a drug, than as a resuscitative solution. In addition to clinical assessment, support with other imaging or invasive techniques is often needed to assess whether volume therapy is adequate. The use of central venous saturation (ScvO2) to assess volume status in patients with ALF, is not applicable, in a similar way to the setting of a hyperdynamic circulation [139]. ScvO2 will be elevated even if the patient is volume depleted and fluid responsive [140]. The purpose of bolus fluid therapy is to increase stroke volume and subsequently, cardiac output. Assessment of an appropriate increase in cardiac output can be achieved with either real time ECG, cardiac or oesophageal Doppler; the latter is only applicable in patients who are ventilated. Use of invasive monitoring (such as pulmonary artery catheter or pulse contour analysis), provides measures of cardiac index. Pulse contour analysis also measures volume status and allows prediction of the likely response to fluid challenge. In ventilated patients use of inspiratory hold can also be used to assess the likely response to volume challenge. Passive leg raise, to investigate for an increase in cardiac output in response to a volume load, is less applicable in the context of high grade HE [141–144]. There are considerable data to suggest that excess fluid and a persistent positive fluid balance is associated with higher mortality in many patient cohorts. Elevated venous pressure can be associated with increased tissue oedema and greater impairment of microcirculatory flow. Elevated right sided cardiac pressures may be detrimental to liver venous outflow and hence liver function and regeneration, gut integrity and renal functions [145– 147]. Therefore, volume overload should be avoided as much as volume depletion. In the cohort of patients with ascites due to subacute liver failure or acute Budd-Chiari syndrome, elevated intraabdominal pressure may be present. This may alter response to volume loading, in addition to increasing risk of gut dysfunction and AKI, response to fluid resuscitation needs to be assessed individually. In patients with elevated right sided cardiac pressures and ascites, further fluid therapy is likely to have limited or minimal effect on cardiac index. Drainage of some ascites may improve venous return and improve cardiac index [148]. Following adequate volume loading, persistent hypotension requires treatment with vasopressors. Given the usual clinical picture in ALF of an elevated cardiac output and decreased vascular tone, the initial pressor recommended would be norepinephrine, at a starting dose of 0.05 lg/kg/min. Additional low dose vasopressin (1–2 units/hour), should be considered if norepinephrine requirements increase to >0.2–0.3 lg/kg/min [149]. More recent studies in critical care sepsis cohorts have not shown any benefit of additional vasopressin [150]. Vasopressin has been suggested to be detrimental in regard to cerebral complications in ALF [151]. However, a study comparing terlipressin and norepinephrine did not show any difference regarding intracranial pressure (ICP) [152]. In patients whose vasopressor requirements are >0.2 lg/kg/min, arterial pressure monitoring from a central artery (axillary or femoral) should be considered, as opposed to a peripheral arterial line in order to ensure accurate measurement. The appropriate blood pressure range to target is highly controversial and largely without evidence. In young patients without pre-existing hypertension, a mean arterial pressure (MAP) of 60 mmHg is more than adequate. In patients who are at risk of AKI there is some evidence that a MAP >75 mmHg may be better in those with chronic hypertension [153]. However, once RRT has been established, there is no evidence to support that maintaining this higher MAP is beneficial [145,154– 156]. Furthermore, other studies have not shown this relationship, and aiming for higher MAP was associated with increased drug related events [157,158]. A recent randomised trial of blood pressure goals failed to demonstrate any benefit for higher perfusion pressures, except in decreasing AKI in those patients with pre-existing hypertension. In those patients where a higher MAP was achieved, there was an increased incidence of atrial fibrillation [156]. Although most patients with ALF will have a hyperdynamic circulation, a proportion of those with hypoxic hepatitis will have evidence of both right and left sided cardiac dysfunction, with or without valvular heart disease. In this setting, optimisation of cardiac function will need to be individualised, regarding volume status and inotropic needs. Right sided pressures should be minimised to facilitate optimal hepatic venous drainage alongside effective left ventricular function. Adequate MAP will need to be achieved with a vasopressor such as norepinephrine, to ensure adequate coronary perfusion pressure. In those with evidence of pulmonary hypertension, specific management is required. A negative fluid balance should be achieved in those with pulmonary venous hypertension or central volume overload. In patients with pulmonary arterial hypertension, control of CO2 is essential and treatment with prostaglandins and sildenafil may be beneficial. Pulmonary artery flotation catheters may be required in combination with cardiac ECG to optimise therapeutic endpoints. Inotropic agents are frequently required; dobutamine or a phosphodiesterase inhibitor such as milrinone, with later administration of levosmendin should be considered. The dosage of such agents requires careful titration in the context of ALF; initiating doses should be very low and without bolus at commencement. In patients with profound and reversible acute cardiac dysfunction, extracorporeal support with venoarterial extracorporeal membrane oxygenation (VA ECMO) may be appropriate [159]. This should only be undertaken in specialised cardiac and liver centres with appropriate expertise. Furthermore, hypoxic hepatitis is a secondary form of ALF and as such, the primary presenting organ failure needs to be addressed and managed to facilitate liver recovery. LTx is not indicated. Whether there is a benefit of giving physiological doses of hydrocortisone to those ALF patients with vasopressor resistant shock is not clear. There are no mortality studies, although there is evidence of adrenal dysfunction in more than 50% of cases with ALF when tested using a standard ACTH stimulation test. One study suggested that use of steroids decreases vasopressor requirements and prolongs time to death, perhaps providing time to obtain a suitable liver for transplantation [160–162]. If this therapy is considered, then potential benefits may be offset by the increased risk of sepsis and reactivation of viral infections (e.g., CMV and herpes simplex virus). If an ACTH stimulation test is undertaken, then a supraphysiological response should lead to the withdrawal of additive steroids as increased mortality has been reported in patients with septic shock [163]. Recent data from the Leuven group provide further insights into adrenal dysfunction in critical illness. Namely, increased cortisol availability appears to be secondary to reduced liver and kidney catabolism [164,165]. A variety of hormonal and hypothalamic-pituitary axis abnormalities can be detected and tracked in critically ill patients, including those with ALF. At present there is a lack of Journal of Hepatology 2017 vol. 66 j 1047–1081 1059 Clinical Practice Guidelines clarity as to the meaning of these measures, and thus far, therapeutic manipulation has not been shown to be beneficial [166– 168]. A study from the USA ALF group has shown that elevated troponin is predictive of poor outcome[169], although a subsequent study did not repeat this finding [170].The observed elevations of troponin are likely to represent myocyte stress in the setting of metabolic disarray and multiple organ failure. Recommendations Most patients are volume depleted at presentation and require crystalloid volume resuscitation (evidence level II-1, grade of recommendation 1). Persistent hypotension requires critical care management, with application of vasopressive agents guided by appropriate monitoring techniques (evidence level II-3, grade of recommendation 1). Norepinephrine is the vasopressor of choice (evidence level III, grade of recommendation 1). Volume overload is as detrimental as underfilling (evidence level II-2, grade of recommendation 1). Hypoxic hepatitis will require consideration of inotropic agents (evidence level II-3, grade of recommendation 1). A blood pressure target has not been defined in the literature (evidence level III, grade of recommendation 2). Hydrocortisone therapy does not reduce mortality but does decrease vasopressor requirements (evidence level II-1, grade of recommendation 1). Considerations for future studies Accurate assessment of volume status with biomarkers for congestion and depletion. Studies of microcirculatory status as an endpoint for resuscitation as opposed to pressures. Appropriate utilisation of VA ECMO in subgroups of patients with ALF and hypoxic hepatitis. Recommendations Standard sedation and lung protective ventilator techniques should be utilised in patients with ALF (evidence level II-3, grade of recommendation 1). Respiratory management Invasive airway management is required in the face of progression to high grade HE to ensure airway protection. In a small proportion of patients with ALF, ventilatory support may also be required for hypoxia and respiratory failure. Non-invasive ventilator support should be avoided in those patients at risk of HE or with profound metabolic disarray, because of the high risk of neurological deterioration, aspiration and poor compliance. 1060 Standard techniques for intubation should be utilised, as guided by specialist critical care societies, with adaptations to account for the brittle haemodynamics and risk of cerebral oedema observed in ALF. Sedation is normally undertaken with a short acting opiate and propofol. Although the latter agent has the potential to decrease blood pressure if the patient is not volume replete, it has beneficial effects with respect to decreasing cerebral metabolic rate for oxygen as well as anticonvulsant properties. Ventilatory settings should be protective; low tidal volume and appropriate levels of positive end expiratory pressure (PEEP) should be utilised to maintain an open lung with low tidal volume [171,172]. Hypercarbia and hypocarbia should be avoided, with CO2 targets of between 4.5 and 5.5 kPa (34–41 mmHg). Tidal volumes should be maintained at 6 ml/kg/ideal body weight, with a maximum of 8. The incidence of acute respiratory distress syndrome (ARDS) or acute lung injury is relatively rare in patients with ALF, and does not appear to contribute to mortality [173]. Care of the airway, appropriate use of physiotherapy and patient positioning should decrease the risk of ventilator associated pneumonia. Secretions should be sampled regularly using non-directed broncho-alveolar lavage, and sent for culture. Ventilator techniques in patients who develop ARDS are beyond the scope of these guidelines. However, there is no evidence to support use of oscillation, and although prone ventilation does improve oxygenation and potentially mortality, its use requires detailed discussion in ALF patients at risk of cerebral complications [174,175]. High levels of PEEP (>12) should be monitored regarding transmitted pressure risk with middle cerebral artery Doppler. The balance of hypoxia, hypercarbia and risk of increased ICP must be individualised at the bedside. In a small cohort, consideration may be given to venous-venous ECMO, with use only being advised in centres with expertise in both ALF and ECMO. Assessment of the aetiology of hypoxaemia can be difficult. In some patients with hypoxic hepatitis there is evidence of hepatopulmonary syndrome [176] and this should be excluded with bubble ECG. In a few cases, there may also be evidence of a toxic liver syndrome with increased lung water and ARDS. Assessment of lung water may facilitate optimal management of these patients. In some patients with significant ascites, the presence of intra-abdominal hypertension may result in significant hypoxia [177], and may be alleviated by limited volume paracentesis. Avoid of excessive hyper or hyocarbia (evidence level III, grade of recommendation 1). Regular chest physiotherapy should be carried out and ventilator associated pneumonia avoided (evidence level III, grade of recommendation 1). Journal of Hepatology 2017 vol. 66 j 1047–1081 JOURNAL OF HEPATOLOGY Consideration for future studies Application of extracorporeal lung support techniques to address risk benefit in highly specific subgroups of patients. Gastrointestinal management Oral nutrition should be encouraged in patients with ALI. Progressive HE or anorexia is likely to result in decreased calorie intake. Consideration may be given to insertion of a nasogastric tube to facilitate enteral feeding. Risk and benefit needs to be assessed at an individual level. The potential risks include causing bleeding during placement and large gastric residue, with microaspiration if HE progresses. Guidance regarding nutritional needs in patients with ALF is largely empirical. Calorie and protein requirements are as per critically ill populations of other aetiologies. Studies suggest predicted calorie requirements are slightly underestimated by standard tools [178–180]. Ammonia monitoring may be useful during commencement of enteral feeding to ensure that there is no associated increase. Failure of gastric emptying may be addressed through placement of a post pyloric feeding tube, but small bowel failure is more difficult to diagnose. Development of ileus and risk of non-occlusive ischaemia may be associated with gut bacterial translocation. The decision to introduce total parenteral nutrition (TPN) should be based upon baseline nutritional status and duration of low calorie intake. Recent studies have not demonstrated any benefit to instituting TPN prior to day 5 to 7 post critical care presentation [181–183]. Patients with ALF have increased resting energy expenditure, which is similar to other critically ill patients. Clinically this is infrequently measured, but has been reported to be increased by 18 to 30% compared with normal controls [184,185]. Early introduction of enteral feeding will minimise loss of muscle mass and reduce the risk of gastrointestinal haemorrhage. A European survey of nutritional support in patients with ALF revealed that 25 of 33 responding units used parenteral nutrition [178]. Lipid emulsions appear safe; LCT/MCT emulsions are the most commonly utilised. In some patients with significant mitochondrial dysfunction, lipid loads will not be metabolised and may accumulate compounding liver injury. This may especially be the case when propofol is utilised in high doses as a sedative agent. Therefore, monitoring of lipid profile along with creatinine kinase is required, targeting serum triglycerides at a concentration <3.0 mmol/L. Furthermore, patients with ALF release free fatty acids into the splanchnic circulation, in contrast with normal controls or patients with sepsis [186]. Profound alterations in circulating amino acids are reported in patients with ALF, characterised by increased tryptophan and its metabolites, aromatic and sulphur containing amino acids and reduced branch chain amino acids leucine, isoleucine and valine. Excessive infusion of amino acids may aggravate the hyperammonaemia that is characteristic of ALF and precipitate cerebral oedema and intracranial hypertension. This may be avoided by regular monitoring of plasma ammonia during both enteral and parenteral nutrition. There is a moderate risk of pancreatitis in patients with acute and hyperacute phenotypes and axial imaging to quantify this may be required if there is clinical suspicion. Management is as per other critical care settings. The finding of severe pancreatitis is a relative contraindication to emergency LTx. Proton pump inhibitors (PPI) are normally administered, although the evidence base for their use is based on risk factors of organ failure and coagulopathy. This, however, should be balanced against the risk of ventilator associated pneumonia and Clostridium difficile infection [187]. PPIs should normally be discontinued when enteral nutrition has been established. Recommendations Patients with ALF have increased resting energy expenditure. Therefore, enteral or parenteral nutrition are warranted (evidence level II-3, grade of recommendation 1). Avoid nasogastric feeding in those with progressive encephalopathy (evidence level III, grade of recommendation 1). Monitor ammonia when instituting enteral nutrition (evidence level III, grade of recommendation 1). PPI administration should be balanced against the risk of ventilator associated pneumonia and Clostridium difficile infection (evidence level II-3, grade of recommendation 1). Consider stopping PPI when enteral feeding has been established (evidence level III, grade of recommendation 1). Consideration for future studies Biomarkers for small bowel ileus and failure. Metabolic management ALF is frequently associated with electrolyte and metabolic disturbances, which are more common in patients with hyperacute ALF, especially when associated with AKI [14]. Hypoglycaemia is a well recognised complication of ALF and is multifactorial in pathogenesis; increased hepatic extraction of glucose, increased hepatic glycolysis and impaired gluconeogenesis, with failure of compensatory renal gluconeogenesis have all been reported [14]. The frequency of hypoglycaemia requiring treatment is increased in patients with paracetamol induced ALF and AKI Journal of Hepatology 2017 vol. 66 j 1047–1081 1061 Clinical Practice Guidelines (55%) compared with patients without AKI (22%) [27,188]. The clinical features of hypoglycaemia may be confused with developing HE. Therefore, frequent monitoring of blood glucose is required in patients with ALF, especially hyperacute cases, where ‘‘BMstix” monitoring should be undertaken every 2 h. Rapid boluses of concentrated glucose may induce large osmotic shifts in intravascular and cerebral compartments and should be avoided, but may be necessary to treat critical hypoglycaemia. Hypoglycaemia is predictive of developing AKI and is associated with increased mortality [189]. Hyperglycemia can exacerbate raised ICP and should be avoided. Tight glycaemic control with infusion of insulin may reduce mortality in the critically ill, with targets of blood glucose between 8.3–10.0 mmol/L (150–180 mg/ dl) [190–193]. However, a recent meta-analysis of patients in neurological critical care suggested outcomes were only improved with higher glucose concentrations (>200 mg/dl; 11.1 mmol/L) as the threshold for insulin administration [194,195]. Hyponatraemia is also relatively common in patients with ALF, especially hyperacute cases. Previously data reported that 32% of cases with paracetamol induced ALF had serum sodium <130 mmol/L [185,197]. There is a correlation between serum sodium and ICP. Infusion of hypertonic saline to maintain serum sodium between 145 and 155 mmol/L compared with standard of care resulted in reduced ICP and less requirement for bolus therapy for sustained episodes of raised ICP. A decrease in vasopressor requirement was also observed during the first 36 h of infusion [198]. These data suggest that hyponatraemia should be avoided, and maintaining relative hypernatraemia with infusion of hypertonic saline can prevent raised ICP. However, serum sodium levels above 150 mmol/L may be associated with cell damage and should be avoided. Therefore, fluid resuscitation and hypertonic saline infusions should be targeted to maintain sodium at 140–145 mmol/L. Rapid change in sodium levels should also be avoided and correction should be correlated to the rate of drop, which should not exceed 10 mmol/L per 24 h [199]. The observed benefits of NAC in ALF may have been attributable to the effect of a sodium load [47,200]. RRT can also be utilised to correct hyponatraemia, facilitate fluid balance and control of acidosis [201]. Acidosis, increased circulating lactate and reduced bicarbonate are common features in patients with hyperacute and acute ALF, and are multifactorial in pathogenesis, with increased systemic production and reduced hepatic clearance reported [131,186,200]. Acidosis is less common in subacute ALF syndromes, possibly due to the alkalinising effect of hypoalbuminaemia [202]. Both acidosis and increased lactate have been proposed as prognostic markers in paracetamol induced ALF. It is likely they are also applicable in other forms of hyperacute liver failure. RRT was utilised in the majority of patients where lactate was identified as an additional possible prognostic marker [130], and therefore RRT should not be withheld when managing patients with ALF or ALI. Alterations in serum phosphate, magnesium, ionised calcium and potassium are commonly observed and should be monitored and corrected, as clinically appropriate. Hypophosphatemia is a favourable prognostic sign and appears to be associated with liver regeneration [203]. Careful replacement therapy is required, however, to avoid the potentially serious organ dysfunction associated with hypophosphataemia. 1062 Recommendations Stringent attention to detail and normalisation of biochemical abnormalities is warranted in patients with ALF (evidence level III, grade of recommendation 1). Hypoglycemia is common in patients with ALF, is associated with increased mortality and needs to be corrected avoiding hyperglycemia (evidence level II-3, grade of recommendation 1). Hyponatreamia is detrimental to outcome and should be corrected to maintain concentrations 140–150 mmol/L (evidence level II-2, grade of recommendation 1). Lactate elevation is related to increased production and decreased clearance, and remains a poor prognostic marker. RRT is indicated to correct acidosis and metabolic disturbances (evidence level II-3, grade of recommendation 1). Acute kidney injury and renal replacement therapy AKI is common in patients with ALF. The two most common classifications are represented by RIFLE and AKIN, but have recently been updated by the Kidney Disease: Improving Global Outcomes (KDIGO) AKI working group [204–206]. The general acceptance of a classification for AKI in patients with ALF will significantly improve studies of epidemiology, prevention and treatment in this context. Revised consensus recommendations for diagnosis and management of AKI in cirrhosis, largely based on KDIGO criteria have recently been proposed by the International Club of Ascites [207]. Their assessment in patients with ALF would be certainly warranted and compared with KDIGO/ADQI for AKI in sepsis and MOF. Between 40 and 80% of ALF patients referred to tertiary liver units are classified as having AKI, which is associated with increased mortality and length of hospital stay. Risk factors for AKI include increased age, paracetamol-induced ALF, hypotension, the presence of the systemic inflammatory response syndrome (SIRS) and infection [197,208]. Strategies to prevent the development of AKI include: correction of hypotension, prompt treatment of infection, avoiding nephrotoxic medications and judicious use of radiological procedures that require intravenous contrast; albeit balancing risks and benefits of contrast radiology and aminoglycosides in any given clinical context. The timing of institution of RRT in the context of ALF has the potential to cause conflict between speciality groups involved in the care for these patients [209]. RRT is normally instituted in the context of uraemia, fluid overload and hyperkalaemia. In the context of ALF, however, RRT may be offered to manage acidosis, hyperammonaemia and sodium imbalance, facilitate temperature and metabolic control and, as such, may be better referred to as liver or metabolic replacement therapy. Slack et al. have shown a clear correlation between creatinine clearance and ammonia clearance [210]. Therefore, early consideration of RRT should be undertaken in those ALF patients with markedly elevated ammonia and, or progressive HE. Journal of Hepatology 2017 vol. 66 j 1047–1081 JOURNAL OF HEPATOLOGY Continuous modes of RRT are preferred to intermittent dialysis. These therapies avoid the large metabolic and haemodynamic fluctuations associated with intermittent dialysis, which could precipitate raised ICP [8,211]. Lactate free buffers accelerate correction of acidosis. Anticoagulation for dialysis is the subject of much debate; options include no anticoagulation, prostacyclin and regional citrate, with little data to recommend which is the safest and most efficacious in patients with ALF. Some data would suggest that although patients with cirrhosis will tolerate citrate anticoagulation, patients with acute and hyperacute ALF may be less able to metabolise the citrate load [212]. If citrate is used in the context of ALF, close monitoring of total calcium compared with ionised calcium is required [213,214]. Most ALF patients with AKI will fully recover renal function either by the time of hospital discharge or following LTx [197]. Predictive factors for complete renal recovery following paracetamol ALF include: female gender, lower model for endstage liver disease (MELD) scores at day 3, patients with admission hypotension and patients with lower grades of AKI [189,208]. Isolated renal failure without ALF is seen in some cases of POD and can normally be managed with intermittent haemodialysis [215]. Recommendations Early institution of extracorporeal support (RRT) should be considered for persistent hyperammonaemia, control of hyponatraemia and other metabolic abnormalities, fluid balance and potentially temperature control (evidence level III, grade of recommendation 1). Anticoagulation of RRT circuits remain a matter of debate, and close monitoring of metabolic status should be undertaken if citrate is utilised (evidence level II-2, grade of recommendation 1). Continuous RRT should always be undertaken in the critically ill patient with ALF as opposed to intermittent haemodialysis (evidence level III, grade of recommendation 1). Considerations for future studies Monitoring and management of anticoagulation of extracorporeal circuits. Appropriate indications for commencing RRT. Biomarkers for the prediction of and recovery from AKI. with ALF. However, this abnormal coagulation is not translated into an increased risk of bleeding [111]. Recent, in depth analysis of coagulation abnormalities in patients with ALF have suggested that most patients have rebalanced haemostasis; most patients have a ‘‘normal coagulation state”, despite prolongation of measured INR or PT, and a significant proportion are hypercoagulable. This is related to significant increases in endogenous heparinoids, procoagulant microparticles, von Willebrand factor and factor VIII, reduced pro- and anticoagulant factors and release of ‘‘younger” more reactive platelets in patients with ALF [112,113,216–218]. Some of these changes may have prognostic significance, but surprisingly there does not appear to be any significant differences between hyperacute and other aetiologies of ALF. Monitoring of coagulation in patients with ALF requires standard and extended laboratory techniques (thrombin generation, factor VIII, etc.) in addition to thromboviscous technology, which should increasingly become a standard additional measure. Appreciation of this balanced haemostasis reinforces the recommendation that prophylactic correction of coagulation or platelet levels is not necessary. It may instead adversely affect prognostication as well as increase the risk of thrombosis or transfusion related acute lung injury in patients with ALF. Arguably there are only two situations that require active management of coagulation and platelets. Firstly, insertion of ICP monitors requires infusion of fresh frozen plasma, cryoprecipitate and platelets depending on the initial assessment of coagulation, as guided by neurosurgical specialist societies. Others have suggested prophylactic recombinant factor VIIa prior to insertion of ICP monitors, but there is no evidence of decreased mortality and a potential significant risk of thrombosis [217–221]. Secondly, significant active haemorrhage necessitates correction of coagulation and thrombocytopenia, in addition to identification and local measures to deal with the source of the bleeding. Although indications in the specific setting of ALF are not available, it seems reasonable to target plasma fibrinogen levels 1.5– 2 g/L by infusing fibrinogen concentrate at an initial dose of 25–50 mg/kg body weight, and a platelet count >60,000/ll [222]. The role of additional supportive therapies such as tranexamic acid should also be considered in this context. An appropriate level of haemoglobin is usually agreed to be greater than 7 g/dl, although adaptation may be considered in the context of severe cardiorespiratory failure or subarachnoid haemorrhage [223]. Recommendations The routine use of fresh frozen plasma and other coagulation factors is not supported, and should be limited to specific situations, such as insertion of ICP monitors or active bleeding (evidence level II-3, grade of recommendation 1). Haemoglobin target for transfusion is 7 g/dl (evidence level II-2, grade of recommendation 1). Coagulation: Monitoring and management Disordered coagulation is an essential diagnostic component of ALF. Rapid changes in the PT or INR are characteristic and of significant prognostic value. Thrombocytopenia, reduced circulating pro- and anticoagulant proteins and increased PAI-1 (favouring fibrinolysis) are all commonly reported in patients Venous thrombosis prophylaxis should be considered in the daily review (evidence level III, grade of recommendation 1). Journal of Hepatology 2017 vol. 66 j 1047–1081 1063 Clinical Practice Guidelines Considerations for future studies Role of anticoagulation to improve microcirculation and decrease liver injury. Further understanding of coagulation disturbances and critically ill patients with ALF and point of care monitoring. Risk of thrombotic complication in the context of ALF and appropriate therapeutic interventions. Sepsis, inflammation and anti-inflammatory management Bacterial, fungal and viral infections: Incidence, timing and nature Patients with ALF are at increased risk of developing infections, sepsis and septic shock. Infectious complications were a leading cause of death in ALF [224–226] although recent data suggest bacteraemia is not independently predictive of mortality [227]. Severe, untreated infection may preclude LTx or complicate the postoperative course. Patients with ALF have multiple immunological alterations [228–230] and an increased requirement for invasive organ support or monitoring, which contributes to colonisation with multi-drug resistant bacteria and the development of nosocomial sepsis. Bacterial infections have been documented in 60–80% of patients; most commonly pneumonia (50%), urinary tract infections (22%), intravenous catheter-induced bacteraemia (12%), and spontaneous bacteraemia (16%). Gram-negative enteric bacilli and Gram-positive cocci are the most frequently isolated [224,225]. More recent data has suggested infection, such as bacteraemia, occur later after admission (median 10 days compared with 3 days in earlier studies), and Gramnegative organisms are now more common isolates than Gram-positive bacteria [227]. Furthermore, recent publications highlight the high frequency of infection with either methicillin resistant Staphylococcus aureus and vancomycin resistant Enterococcus [227]. Fungal infections occur in about one-third of patients requiring prolonged critical care support with ALF, largely with candida species. These patients frequently have concurrent bacterial infection. Viral infections and reactivation of CMV is common in critically ill patients [231,232] and is likely to be present in ALF, albeit poorly reported in the literature. Absolute attention to hand washing, and care of extraneous monitoring devices such as urinary catheters, venous and arterial cannulae and appropriate bronchial toilet are essential. Strict asepsis should be utilised when lines are manipulated. Diagnosis of infection The diagnosis of infection in patients with ALF is difficult; the clinical features are non-specific and examinations such as C reactive protein and procalcitonin measurements are frequently unhelpful. A high level of clinical suspicion of infection should be maintained in patients with ALF [233,234]. Routine microbi- 1064 ologic surveillance can result in early detection and treatment of infections [224]. Admission and frequent screening of blood, urine and appropriate samples for cultures should be performed as clinically indicated. Admission HE and SIRS score >2 are significant predictors of bacteraemia, and deterioration of mental status, unexplained fever and leukocytosis (particularly in patients with paracetamol toxicity), may represent the onset of infection [227]. Deterioration in hepatic coma grade after initial improvement, pyrexia unresponsive to antibiotics, established renal failure, and marked elevation in white cell count should prompt aggressive investigation for fungal, bacterial or viral infection. This is especially important in patients already on broad spectrum antibiotics. Use of biomarkers for fungal infection should be utilised, whilst recognising their high false positive rate, but low risk of false negative results [235]. Treatment vs. prophylaxis and infection control standards Broad spectrum antibiotics are generally used to cover common organisms such as Staphylococcal species, Streptococcal species, or Gram-negative rods. Empirical broad spectrum antibiotics should be administered to patients with ALF who have signs of SIRS, refractory hypotension or unexplained progression to higher grades of HE [10]. Prophylactic parenteral antimicrobial therapy reduces the incidence of infection in certain groups of patients with ALF. However, survival benefit has not been shown [236]. Selective bowel decontamination using non-absorbable antibiotics and parenteral antibiotics also do not impact survival [237]. An association of infection and SIRS with progression to deeper stages of HE has been reported [226,238], and a reduction of infection and SIRS may have an impact on ICP [239–241]. However, there are no controlled trials confirming that the use of prophylactic antimicrobials decreases the likelihood of progression of HE or the development of raised ICP. Therefore, there is not sufficient data to support a generalised antibiotic prophylaxis practice in ALF [236]. Empiric antibiotics are recommended for patients listed for super urgent LTx, since the development of infection and sepsis may prompt delisting. Decisions surrounding antimicrobial choice should be based on knowledge of local microbiological data. Association of SIRS and organ dysfunction ALF is associated with dynamic immune dysfunction. An altered balance between opposing systemic pro- and antiinflammatory immune profiles can contribute to organ failure and death in ALF, irrespective of aetiology [44,228,239,242– 247]. Liver injury due to any type of insult leads to: the activation of the innate immune system, altered macrophage function, impaired neutrophil function, initial activation of the complement system (and thence marked reduction in complement levels), impaired phagocytosis and opsonisation resulting in functional immunoparesis. Liver cell death leads to a release of pro-inflammatory mediators, which may be associated with elimination of pathogens and tissue regeneration. However, they may also be associated with the Journal of Hepatology 2017 vol. 66 j 1047–1081 JOURNAL OF HEPATOLOGY mediation and propagation of further tissue damage. Local tissue injury and inflammatory responses are associated with a ‘‘spill over” phenomenon of chemotactic mediators and proinflammatory cytokines, which subsequently leads to the recruitment of monocytes, lymphocytes, and polymorphonuclear leukocytes [218,248–252]. These cells secrete vasoactive mediators, which activate both platelets and the coagulation cascade, and further increase vascular permeability alongside microcirculatory failure and thrombosis [113,218]. This process leads to SIRS. Release of damage associated molecular patterns, e.g., HMGB1, from injured hepatocytes may also contribute to the development of SIRS [246]. SIRS leads to a vicious cycle wherein an increase in vascular permeability further contributes to tissue injury. Over time, the balance tilts towards the anti-inflammatory response, which is associated with immune suppression, recurrent infections, sepsis, and death [243]. SIRS appears to be involved in the worsening of HE, reduces the chances of transplantation and confers a poorer prognosis, independent of infection [44,226]. In a timecourse study, the appearance of SIRS occurred earlier and with a greater magnitude in patients with severe paracetamolinduced hepatotoxicity who died, compared with surviving patients [253]. Similarly, the development of SIRS preceded the development of organ failure, and increased SIRS scores was associated with increased SOFA scores and risk of mortality [208,254]. There is an association between infection and SIRS. Early studies suggested infected patients were more likely to develop SIRS, and the extent of their physiological disturbance was greater than that of uninfected patients, although recent publications question this [227,238]. Arterial lactate levels correlate with the SOFA score and the number of SIRS components [253]. Inflammation also plays a synergistic role in the pathogenesis of high grade HE and raised ICP because of its effects on cerebral blood flow (CBF) and activation of brain inflammation [255–259]. Inflammatory markers, arterial ammonia, and CBF were higher in patients with poor prognosis, and TNFalpha levels correlated with CBF [238]. Inhibition of brain inflammation in animal models results in decreased brain water and reduced ICP [260–262]. Potential biomarkers in ALF: Cytokines, HLA-DR, and cell death serum markers There is still a need to identify ALF-specific and dynamic biomarkers that can be used for follow-up and for determining outcome. Expression of HLA-DR and markers of apoptosis have been suggested as biomarkers of ALF. The percentage of monocyte HLA-DR expression is lower in patients with ALF when compared to healthy volunteers or patients with chronic liver disease. It correlates with INR, blood lactate, pH, and levels of encephalopathy, predicting poor prognosis [241,263] as do markers of inflammation and coagulation [264,265]. The measurement of caspase-cleaved and uncleaved cytokeratin-18 is an early predictor of survival in severe septic patients with hepatic dysfunction [249,266]. Patients who spontaneously recover from ALF revealed a significantly higher level of activation of caspases than those who required transplantation or died [267,268]. Acetylated HMGB1 secreted from activated macrophages may also aid in prognostication [248,269]. Recommendations Prophylactic antibiotics, non-absorbable antibiotics, and antifungal have not been shown to improve survival in ALF (evidence level II-2, grade of recommendation 1). Regular periodic surveillance cultures should be performed in all patients with ALF (evidence level III, grade of recommendation 1). Early anti-infection treatments should be introduced upon appearance of progression of hepatic encephalopathy, clinical signs of infections, or elements of SIRS (evidence level II-3, grade of recommendation 1). Antifungal therapy in those with prolonged critical care support for multiple organ failure should be considered, as guided by the use of biomarkers (evidence level II-3, grade of recommendation 1). Considerations for future studies Integration of inflammatory biomarkers with biochemical and functional markers of liver function. Biomarkers to separate infection and inflammation. Immunomodulatory therapy to promote liver regeneration and decrease nosocomial sepsis. The brain in ALF Neurological manifestations HE is an essential manifestation of ALF, characterised by a decrease in the level of consciousness and altered neurotransmission. HE tends to fluctuate and may progress from a trivial lack of awareness to deep coma. Additional manifestations may include headache, vomiting, asterixis, agitation, hyperreflexia and clonus [196]. The diagnosis of HE is clinical and requires the exclusion of other causes of neurological disturbance (e.g., hypoglycemia, hypercapnia, non-convulsive seizures, stroke, encephalitis, effect of sedatives and other causes). One characteristic manifestation of ALF is the development of clinically significant brain oedema and intracranial hypertension (ICH). These can manifest as a result of arterial hypertension, bradycardia and mydriasis in patients who have progressed to grade 3 or 4 coma. The course of HE is dictated by the outcome and phenotype of liver failure, and usually parallels the evolution of other parameters of liver function. Additional factors that may worsen the neurological outcome are the coexistence of infection or presence of inflammation without sepsis alongside the presence of other organ failure [8,226,255,259,270]. Principles of care for patients with a low level of encephalopathy Regular clinical and mainly neurological examination is mandatory in order to detect early signs of HE and progression to high Journal of Hepatology 2017 vol. 66 j 1047–1081 1065 Clinical Practice Guidelines grade encephalopathy (grade 3 and 4). Patients should be managed in a quiet environment with regular monitoring and management of other parameters, with especial attention directed to serum sodium as previously discussed. Although ammonia reducing strategies may be of benefit, the role of conventional treatments for HE (lactulose and rifaximin) have no evidence base in ALF. Lactulose may be associated with increased risk of ileus and bowel dilation. Management of the patient with altered Glasgow Coma Scale (GCS) Once the patient progresses to grade 3 HE, the general practice at transplantation centres is for intubation and mechanical ventilation; measures that protect the airway prevent aspiration and provide safer respiratory care [10]. Grade 3 coma, in the context of ALF and its management, is not defined by a hepatic flap but the development of marked agitation and frequent aggression with a decrease in GCS (GCS usually E1-2, V 3-4 and M4). Progression to grade 4 coma is associated with marked reduction in GCS (E1, V 1-2 and M1-3) [14]. Ventilatory management, specifically related to cerebral protection, includes: minimising the risk of pulmonary barotraumas, aiming for a partial pressure of carbon dioxide (PaCO2) between 4.5–5.5 kPa (34–42 mmHg) and use of propofol as a sedative agent. This may protect from ICH and reduce the risk of seizures [271]. A short acting opiate should be added to provide adequate analgesia. In case of concern of seizure activity, EEG monitoring should be undertaken and antiepileptic drugs administered; however, the prophylactic use of antiepileptic drugs is not warranted [272]. Phenytoin has traditionally been the medication of choice; however, agents without risk of hepatotoxicity and more easily achieved therapeutic levels such as levetiracetam or lacosamide are now more frequently utilised. Intracranial hypertension Brain oedema that causes ICH is a classically described complication of HE in ALF. Though the incidence of ICH has decreased recently, it still may affect one-third of cases who progress to grade 3 or 4 HE [8]. Patients at a higher risk of ICH are those with a hyperacute or acute phenotype, that is a shorter jaundice-toencephalopathy interval [4], younger age (likely related to decreased available free space within the cranium), renal impairment (associated with increased ammonia and an inflammatory phenotype) and need for inotrope support (frequently associated with an inflammatory phenotype [259]. Persistent elevation of arterial ammonia (>200 lmol/L) levels, especially following initial management, also indicate an increased risk of ICH [259,273,274] whilst decreasing values represent a lower risk [275]. The physical signs defined at clinical examination (pupil dilation, fixed or sluggish response to light and sustained hypertension) are not sensitive enough to predict changes in ICP. Brain imaging may be more reliable, but CT scans are relatively insensitive to actual ICH and moving patients with severe HE can lead to surges of ICP. For this reason, scans are not recommended for monitoring brain oedema and are reserved for diagnosing intracranial bleeding or cerebral herniation with absent perfusion. ICP monitoring provides the gold standard for measurement and monitoring of ICP and hence management of pressure 1066 surges. However, its use does not seem to modify patients’ outcomes [220,276,277] and is associated with clinical risk, since bleeding within the cranium combined with brain oedema can lead to significant morbidity and mortality. Therefore, placement of ICP devices remains a matter of intense debate, with their use reserved for patients at high risk of ICH, and in centres with large neurosurgical experience in ALF management [278–280]. Several non-invasive techniques have been proposed to estimate ICP, but all are complex and demonstrate considerable ‘‘inter and intra-assay” variability. Changes in CBF reflecting ischaemia and vasodilation of the cerebral circulation and resistance to flow, with increased ICP, can be assessed using middle cerebral artery Doppler [281]. An increase in CBF usually precedes the rise of ICP. Indirect data can be obtained by monitoring reverse jugular vein oxygen saturation; values over 80% usually indicate hyperaemia and under 55% relative ischaemia. The latter suggests a scenario where cerebral oxygen consumption is in excess of supply due to epileptiform activity (increased demand) or inadequate supply (hyperventilation and hypocapnia, inadequate blood pressure or cardiac index). The measurement of optic nerve depth is also representative of ICP, according to a recent assessment [282]. Therapeutic options for raised intracranial pressure General measures include elevation of the head at a 30-degree upright angle, avoidance of fever, hypoglycaemia or hyperglycemia and clamping of serum sodium at 140–145 mmol/L. In patients who are monitored for ICP, pressure should be maintained below 20–25 mmHg and the difference between MAP and ICP (cerebral perfusion pressure, CPP) should remain above 50 mmHg [283]. However, in all such clinical scenarios, individualised treatment must be implemented because an increase in MAP is often associated with an increase in CBF and hence ICP. As a result, survivors with protracted low CPP have been reported [284]. Sustained surges in ICP (>25 mmHg) or development of clinical signs should be treated by a bolus of hypertonic saline (200 ml, 2.7% or 20 ml, 30%) [199] or intravenous mannitol (150 ml, 20%) given over 20 min [285], in addition to ensuring optimal sedation. In a resistant scenario, a short period of hyperventilation may be required, reducing arterial PaCO2 to 25–30 mmHg. Steroids are not recommended [285]. It is essential that serum osmolarity is maintained below 320 mOsmol and RRT may frequently be required to facilitate this. In situations where the patient has cerebral hyperaemia and signs of ICH persist despite mannitol and hypertonic saline, a bolus intravenous indomethacin may be considered (0.5 mg/kg) [286]. L-ornithine L-arginine has not been shown to be beneficial [287]. Mild hypothermia may be effective for uncontrolled ICH [288,289], but other critical care literature reports that although hypothermia decreases ICP there is no beneficial effect on mortality [290]. Hepatectomy is a theoretical possibility as a bridging procedure to LTx for those patients with devastating and medically uncontrolled ICH in whom there is perceived to be no chance of spontaneous survival [291]. Journal of Hepatology 2017 vol. 66 j 1047–1081 JOURNAL OF HEPATOLOGY Recommendations Patients with low grade encephalopathy should be frequently evaluated for signs of worsening encephalopathy (evidence level III, grade of recommendation 1). In patients with grade 3 or 4 encephalopathy, intubation should be undertaken to provide a safe environment and prevention of aspiration. Regular evaluation for signs of intracranial hypertension should be performed (evidence level III, grade of recommendation 1). Trans-cranial Doppler is a useful non-invasive monitoring tool (evidence level II-3, grade of recommendation 1). Invasive intracranial pressure monitoring should be considered in a highly selected subgroup of patients, who have progressed to grade 3 or 4 coma, are intubated and ventilated and deemed at high risk of ICH, based on the presence of more than one of the following variables: a) young patients with hyperacute or acute presentations, b) ammonia level over 150–200 lmol/L that does not drop with initial treatment interventions (RRT and fluids), c) renal impairment and d) vasopressor support (>0.1 lg/kg/min) (evidence level II-3, grade of recommendation 1). Mannitol or hypertonic saline should be administered for surges of ICP with consideration for short-term hyperventilation (monitor reverse jugular venous saturation to prevent excessive hyperventilation and risk of cerebral hypoxia). Mild hypothermia and indomethacin may be considered in uncontrolled ICH, the latter only in the context of hyperaemic cerebral blood flow (evidence level II-2, grade of recommendation 1). Considerations for future studies Accurate non-invasive assessment of ICP should be developed and validated. Relationship irritation. between inflammation and cerebral Modulators of cerebral inflammation need to be studied. Artificial and bioartificial liver devices Liver assist devices have received much attention over recent years in the hope that they can provide an effective ‘‘bridge” to transplantation or recovery of liver function, mitigating the need for transplantation. Unfortunately, the dream of a mechanical ‘‘proxy liver” is a long way from being realised. Preliminary artificial liver support devices were essentially filters designed to remove toxins through haemodialysis or adsorption using charcoal, and failed to show a survival benefit in ALF [292,293]. In the future, it will be essential to learn the lessons of the past, i.e., that case series always seem to show benefit, whilst well-designed clinical randomised controlled trials (RCTs) often fail to fulfil the hopes of initial reports. The Molecular Absorbent and Recirculating System (MARSÒ) system utilises a hollow fibre, double-sided, albuminimpregnated dialysis membrane, designed to extract proteinbound toxins into the albumin dialysate [294]. Initial reports suggested improvements in both systemic and cerebral haemodynamic parameters and improvements in HE in patients with ALF [295–297]. The PrometheusÒ system, which separates plasma and treats it over adsorbent columns, has reported benefit in AoCLF but has not been studied in ALF [298,299]. At least 12 RCTs of these devices have been performed and have been systematically reviewed several times; overall, these devices improve HE but have no mortality benefit in ALF, nor do they show benefit in AoCLF [300,301]. The most recent trial from France examines ALF treated with the current care standard or MARS. Overall there was no mortality benefit, although a trend for improved survival was seen in non-transplanted patients with paracetamol induced hepatotoxicity [302]. Two factors should be considered in assessing the outcome from this study. Firstly, that although paracetamol induced hepatotoxicity is an aetiology with gross physiological disarray, these patients have the best chance of spontaneous survival. Secondly, that the median time to LTx in this study was 16 h, with a median of 1 MARS treatment prior to LTx. Therefore, it would be unrealistic to expect any system to have an impact on mortality over such a short period. Subgroup analysis suggested a trend to better outcome in those who received three treatments. The biological systems of artificial liver support are more complex, but allow the opportunity to facilitate both clearance and metabolism of toxins, and support of hepatocyte function. These may be divided into whole organ perfusion (human or xenoperfusion), hepatocytes (porcine or hepatoblastoma) presented on columns and perfused following plasma separation, and transplantation of either hepatocytes or stem cells. In case series, the original system of porcine hepatocytes and charcoal adsorbents (BAL) showed benefit in measured physiological parameters, biochemical variables and ICP [303,304]. Unfortunately, the subsequent RCT, including patients with primary graft non-function, failed to show improvement in terms of mortality or neurological outcome and complications [304]. There has been an increasing concern raised in utilising xenoperfusion techniques, due to the potential risk of viral transmission. Artificial bioreactors have therefore moved towards incorporating hepatocyte and hepatoblastoma cell lines. Biomedical engineering of these systems has developed vastly over the last 20 years and continues to rapidly evolve. The Extracorporeal Liver Assist Device (ELADÒ) system, which utilises hepatoblastoma cell lines, has been studied in various contexts and shows some benefit in physiology and biochemical parameters [305]. However, it has failed to show a mortality benefit in ALF. This system provides a greatly increased hepatocyte mass, and a RCT in AoCLF and ALF patients is in progress. The opportunity for hepatocyte or stem cell transplantation remains an exciting proposition. Case series in children suggests a benefit, especially to metabolic disease states. Further studies Journal of Hepatology 2017 vol. 66 j 1047–1081 1067 Clinical Practice Guidelines are needed to examine the opportunities in adults with ALF, although the potential could be limited by the volume of cells required. Clarification as to the most appropriate site and mode of cell delivery will also require investigation [306,307]. Plasma exchange (PE) in patients with ALF, undertaken on the first 3 days of admission to critical care, has been shown to have physiological and biochemical benefits, and to decrease ICP in case series [308,309]. A recently published RCT in which PE was undertaken, replacing plasma with fresh frozen plasma on a 1:1 ratio, demonstrated a mortality benefit in patients with ALF who did not undergo transplantation. The survival benefit was also seen in those who fulfilled poor prognostic criteria but who were not listed due to co-morbidity. Furthermore, PE appears to modify monocyte immune function, offering putative rationale for survival benefit, in addition to the immediate clearance of mediators and replacement of plasma derived factors [310]. Despite all these liver assist systems, the emphasis must remain on provision of high general standards of critical care. Physiological derangement in ALF can often be appropriately managed with the organ support techniques described previously, including consideration for the use of beta blockers, as suggested by a recent study [311]. Biochemistry can also be improved by appropriate fluid resuscitation and RRT, both of which have been shown to decrease bilirubin and ammonia [312]. All the devices described above are likely to affect clearance of antimicrobial drugs and sedatives. Therefore, consideration must be given to appropriate dosing schedules [313,314]. Anticoagulation of artificial circuits is variable and, as with RRT, a variety of solutions may be considered. These should recognise that patients with ALF will be resistant to heparin effects related to low anti-thrombin III levels, and may have issues with citrate [212,315,316]. One of the challenges in assessing the efficacy of liver assist devices is that many of the prognostic markers of liver function, which are used to assess clinical course, may be modulated by the liver systems being studied. This is particularly the case for such systems as PE, affecting coagulation, ammonia and bilirubin; adsorbent systems affect bilirubin and ammonia, biological systems and potentially coagulation. The clinical skill will be to recognise and separate liver recovery and regeneration from the effect of any liver support system, and to make the subsequent decisions as to whether LTx or other medical treatment is needed. Recommendations Liver support systems (biological or adsorbent) should only be used in the context of RCT (evidence level II-1, grade of recommendation 1). Plasma exchange in RCT, has been shown to improve transplant-free survival in patients with ALF, and to modulate immune dysfunction (evidence level I, grade of recommendation 1). Plasma exchange may be of greater benefit in patients who are treated early and who will not ultimately undergo LTx (evidence level I, grade of recommendation 2). 1068 Considerations for future studies Well-designed RCT of new liver support systems in welldefined patient cohorts. Development of dynamic measures of liver function to assess metabolic and synthetic capacity. Antimicrobial clearance and dosing when utilising various liver support systems such as PE. Liver transplantation The use of LTx has been the most significant development in the treatment of ALF in 40 years and has transformed survival [8,15]. One year survival following emergency LTx is slightly worse than for routine transplants, but stands at an impressive 80%. The selection for LTx not only depends upon accurate prediction of survival without transplant, but also requires consideration of the survival potential after LTx, and whether a patient is too sick to transplant [317]. Assessment and prognosis Early recognition of patients who will not survive with medical therapy alone is of great practical importance to identify potential candidates for LTx. As progression of MOF results in many patients deteriorating whilst awaiting a transplant, identification of candidates for transplantation should be achieved as quickly as possible. Prognostic assessment should take place both in the transplant centre and the site of first presentation, as decisions related to patient transfer and LTx must be made at the earliest opportunity. A low threshold must be maintained for discussion in relation to management. Clinical features indicative of poor prognosis Even at an early stage of disease, there may be apparent clinical features that are highly suggestive of an expected poor survival with medical management alone, and may be used for risk stratification. Encephalopathy. The presence of an altered level of consciousness resulting from HE is of great prognostic importance. The central positioning of HE in definitions of adult ALF reflects this, with development indicating critically impaired liver function. In patients with subacute presentations, even low grade HE may indicate extremely poor prognosis, whereas survival with medical management may be good in hyperacute disease and HE of equivalent severity. Adoption of a single threshold of HE severity to mark transition from liver ‘‘injury” to ‘‘failure” across all presentations and etiologic groups is thus overly simplistic; the lack of agreed definitions complicates the literature. However, as a rule, any evidence of HE should prompt local critical care assessment, discussion and transfer to a specialist liver centre. When multiple possible causes of reduced consciousness exist, a significantly elevated arterial ammonia concentration is a reliable indicator of HE. Journal of Hepatology 2017 vol. 66 j 1047–1081 JOURNAL OF HEPATOLOGY Extrahepatic organ failure. Non-liver organ failure, particularly renal, is a marker of illness severity and associated with increased mortality [44,209,267]. It indicates need for critical care review and intervention and should trigger discussion with a specialist centre in relation to management and possible transfer. Adverse aetiology and presentation. Even now, subacute presentation of ALF and cases of indeterminate aetiology have consistently poor survival without LTx, and represent triggers for immediate discussion with a specialist centre [9,93]. Severity of liver injury. In patients without HE, progression of disease is more likely in conjunction with major liver dysfunction. In those with established ALF, poor prognostic criteria are more likely to be fulfilled with a need for transplantation in patients with significant liver injury. Whilst laboratory parameters of coagulation disturbance are of prognostic significance in all causes of ALF, the thresholds triggering clinical concern vary by aetiology, evolution of the condition and age of the patient. For example, an INR of 2.5 would be of immediate concern in subacute ALF but not in paracetamol related disease; a factor V level <20% may indicate a poor prognosis in patients of 30 years or younger, but a higher threshold of <30% is of equivalent significance in older patients [318–320]. Another issue is the lack of a consistent international measure of coagulation, with considerable variation in the frequently reported INR measure. Some consistency may be achieved with reporting of PT and control values. The significance of specific biochemical markers of liver injury may also vary by aetiology. Bilirubin level, for example, is not of prognostic value in patients with paracetamol related disease but is a key predictor of outcome in many cases with nonparacetamol causes, especially in subacute and acute presentation [321,322]. Transplantation selection criteria Worldwide, different prognostic evaluation systems to select candidates for transplantation are in use. These utilise features associated with poor prognosis derived from analyses of historic patient cohorts managed with and without transplantation [267,274,318,321,322]. Whilst details differ, they share common features (Table 11A). The presence of HE is a key indicator, with further consideration of patient age and liver injury severity assessed by the magnitude of coagulopathy or jaundice. In general, falling transaminases, increasing bilirubin and INR and shrinking liver are poor prognostic signs and should result in considering transfer of patient to a transplant centre. Although in active and apparently successful clinical use, published data on the performance of the selection criteria are scant, and no system has been universally adopted. The two most commonly used systems in Europe are the Kings College and the Clichy criteria (Table 11B). Of these, the performance of the Kings College criteria are best characterised; meta-analyses confirm clinically acceptable specificity, but more limited sensitivity [263,324,325]. A recent report of the performance of the Clichy criteria suggested a reduced sensitivity and specificity, which could be improved by separating paracetamol and nonparacetamol cases as well as including bilirubin and creatinine clearance in the model [20]. Furthermore, the UK has recently modified the national transplant listing criteria, increasing the threshold for concentrations of lactate in paracetamol induced ALF and allowing listing of subacute cases with predicted poor prognosis without HE [317]. With improvements in medical supportive care in some aetiologies of ALF, particularly paracetamol induced disease and other hyperacute aetiologies, a greater proportion of patients will now survive spontaneously. Thus, prognostic systems calibrated from patients treated decades ago may no longer be appropriate. Studies report evidence of increasingly poor performance over time [263,325]. To address these limitations, a wide variety of alternate prognostic systems and markers to replace or supplement existing criteria have been proposed (Table 12). These include the use of routine laboratory measures, including specific measures such as blood lactate or phosphate, or composite laboratory measures such as the MELD score [203,230,246,322]. Novel replacement criteria include those based upon routine laboratory measures and clinical findings, and those utilising novel markers of immune activation or liver cell injury [240,246,248,267]. Additional proposed indicators of liver dysfunction include those which dynamically assess hepatic metabolism of marker substances, including indocyanine green, galactose or methacetin [326–331]. Many new marker studies report better diagnostic performance than existing criteria but are often small in size, have limited methodological quality and are seldom internally or externally validated. Consequently, few (if any) have been adopted internationally and cannot be recommended for routine use. Recommendations Prognostic assessment should take place not only in the transplant centre but also at the site of first presentation, as decisions in relation to patient transfer to a specialist centre must be made at the earliest opportunity (evidence level III, grade of recommendation 1). Development of encephalopathy is of key prognostic importance, with onset indicating critically impaired liver function. In subacute presentations, even low grade encephalopathy may indicate extremely poor prognosis (evidence level II-2, grade of recommendation 1). Prognosis is worse in patients with more severe liver injury, extrahepatic organ failure and subacute presentations (evidence level II-3, grade of recommendation 1). Transplantation should be considered in those patients fulfilling Clichy or Kings College criteria (evidence level II-2, grade of recommendation 1). Considerations for future studies Future studies should prospectively assess the current natural history of the condition, be of high methodological quality and sufficient size, enrolling from multiple centres. Future studies should avoid the assumption that transplantation equals non-survival for prognostic modelling purposes. Journal of Hepatology 2017 vol. 66 j 1047–1081 1069 Clinical Practice Guidelines Table 11. (A) Acute Liver Failure Poor Prognosis Criteria in use for selection of candidates for Liver Transplantation. (B) Criteria for emergency liver transplantation. A Factor Clichy [323] Kings College [321] Japanese [6] Agey Aetiology Encephalopathyy Bilrubin* Coagulopathyy + + + + + + ± + + + + + B King’s College criteria ALF due to paracetamol Arterial pH <7.3 after resuscitation and >24 h since ingestion Lactate >3 mmol/L or The 3 following criteria: o Hepatic encephalopathy >grade 3 o Serum creatinine >300 lmol/L o INR >6.5 ALF not due to paracetamol INR >6.5 or 3 out of 5 following criteria: o Aetiology: indeterminate aetiology hepatitis, drug-induced hepatitis o Age <10 years or >40 years o Interval jaundice-encephalopathy >7 days o Bilirubin >300 lmol/L o INR >3.5 Beaujon-Paul Brousse criteria (Clichy) y * Confusion or coma (hepatic encephalopathy stage 3 or 4) Factor V <20% of normal if age <30 year or Factor V <30% if age >30 year Factors common to all prognostic models. Bilirubin not included in paracetamol criteria. Liver transplantation: Ethical issues, initial postoperative period and outcome Who to transplant: Ethical issues One of the key issues for ALF is to determine those patients who will die, and those who will spontaneously survive without LTx. Thus, criteria for the indications of emergency LTx are mandatory. In addition, these criteria are needed early in the disease course, in order to have time to find a suitable donor should LTx be required. Psychological assessment of the patient is frequently difficult in the time frame available, due to the emergency context and the presence of HE. In this context, the decision to transplant or not is based on specific issues such as expected compliance, familial status or environment. In addition, some causes of ALF commonly affect patients considered at risk for non-compliance with medication and hospital attendance. As an example, acute hepatitis B can be the consequence of intravenous drug use. Some patients may have a history suggestive of other substance dependency, albeit not responsible for the liver failure. During decision making, several factors should be taken into account: the age of the patient, past history of suicide attempts, and absence of compli- 1070 ance with any previous medical treatments. It is essential to obtain information from the family and friends of the patient, family doctors, psychiatrists and to solicit input from all members of the multidisciplinary team. In ALF, some classical contraindications to LTx in chronic liver disease might be set aside, such as suicide attempt, current consumption of alcohol or drug-addiction and chaotic psychosocial life. Thus, the decision to transplant or not based on psychosocial factors, is complex and requires clear documentation and rationale. However, the long-term outcome is favourable with high levels of treatment compliance [332]. There is likely considerable variation from centre to centre and country to country. In all cases, major efforts should be undertaken to reconstitute the medical and psychosocial environment of the patient and ensure psychosocial support whether the patient undergoes LTx or not. Contraindication to transplantation may also be determined by: physical health issues, age, cardiac and respiratory disease, recent malignancy, pancreatitis and severe sepsis, unresponsive to treatment. Timing and decisions The prognosis of ALF has recently improved and several centres have suggested that early referral is an important reason for this Journal of Hepatology 2017 vol. 66 j 1047–1081 JOURNAL OF HEPATOLOGY Table 12. Comparison of traditional criteria for emergency liver transplantation compared with new alternatives. Prognostic variable Aetiology Predictor of poor prognostic outcome Sensitivity Specificity KCC Clichy criteria All All Factor V; factor VIII/V ratio Paracetamol Phosphate APACHE II Gc-globulin Paracetamol All All 69 86 91 91 89 68 73 30 92 76 91 100 100 87 68 100 Lactate Paracetamol 81 95 a-Fetoprotein MELD Paracetamol Paracetamol Non-paracetamol See Table 5 HE + Factor V <20% (age <30 yr) or <30% (age >30 yr) Grade III-IV HE + Factor V <20% Factor VIII/V ratio >30; Factor V <10% PO3 4 >1.2 mmol/L on day 2 or 3 post overdose APACHE II >19 Gc-globulin <100 mg/L Paracetamol Non-paracetamol Admission arterial lactate >3.5 mmol/L or >3.0 mmol/L after fluid resuscitation AFP <3.9 lg/L 24 h post peak ALT MELD >33 at onset of HE MELD >32 100 60 76 74 69 67 KCC, King’s College Hospital; APACHE, Acute Physiology and Chronic Health Evaluation; MELD, Model for end-stage liver disease. observation. Indeed, this gives time to prevent progression of ALF and to stabilise the patient prior to transplantation, in those who fulfil poor prognostic features. In most European countries, patients with criteria for LTx are on a transplant waiting list, which gives the patient an absolute priority over other cases. As and when a liver graft becomes available, the patient should be re-assessed for their suitability to proceed regarding physiological status or improvement to the point where LTx is no longer considered appropriate. In the context of living related donation, LTx should not be undertaken without progression to poor prognostic criteria, in the same manner as cadaveric grafting [333]. When a patient is too sick for liver transplantation The only definitive criteria contraindicating LTx is irretrievable brain injury. This is normally defined as the persistent presence of bilateral non-reactive pupils with no spontaneous ventilation, loss of middle cerebral artery flow or loss of grey white matter differentiation and evidence of uncal herniation. Bacteraemia, present in 20–30% of patients, is not a contraindication to transplantation providing there is appropriate response to treatment. Progressive vasoplegic shock with rapidly rising vasopressor requirement and peripheral vascular failure would be considered a relative contraindication to proceeding, as would severe haemorrhagic pancreatitis and extensive small bowel ischaemia. Uncontrolled ARDS and haemorrhagic pancreatitis are also relative contraindications, as would be the finding of a markedly low cardiac output state. Relative change, as opposed to absolute values of prognostic variables, will inform the decision to proceed to LTx. This decision should involve all members of the multidisciplinary team. Type of graft The main particularity of LTx for ALF is the context of emergency. Therefore, the possibility of choosing the best graft is frequently reduced, due to shortage of time. The classical procedure when performing LTx is orthotopic LTx using a liver graft from a cadaveric donor. This approach is possible due to the high priority of such patients on the waiting list in most countries. In many countries, it is therefore possible to transplant the ALF patient within 72 h of adding the patient to the waiting list. However, due to the urgency, it is frequently necessary to use marginal donors: aged donors or steatotic grafts. It has been shown that the use of these high-risk grafts might have a deleterious impact on post-transplant outcome and survival [16]. Due to the emergency context, the use of ABO incompatible grafts has been advocated. The successful use of ABO incompatible graft is possible but at a much higher risk of severe rejection, infectious complications and of mortality or retransplantation [334,335]. Other factors associated with poorer outcome are age (>45 years) and vasopressor use. However, outcome has also improved over time [16,336,337]. An interesting approach based on the potential regeneration of the liver is auxiliary orthotopic liver graft (APOLT). The principle is to leave part of the native liver by performing a partial hepatectomy and transplanting a partial liver graft from a cadaveric donor in an orthotopic position [338]. Thus, the graft is supposed to act as a bridge in helping the patient to survive the period of ALF, until potential regeneration of the native liver. If the liver function of the native liver returns to normal, then it is possible to slowly and progressively reduce the immunosuppression, leading to progressive graft atrophy [339,340]. This strategy is potentially more challenging, with an increased risk of bleeding and more frequent post-transplant complications. The overall survival is lower than for orthotopic LTx. Regeneration of the native liver does occur in a significant proportion of cases, but can take prolonged periods of time to complete [341]. Therefore, the indications of APOLT are limited to patients with a high potential of liver regeneration, young patients, patients with ALF due to hepatitis A or paracetamol poisoning. It is not appropriate in patients with severe grade HE and high risk of brain death. Living donor LTx is rarely used in Europe and USA due to the rapid availability of cadaveric liver grafts. In addition, it can place high emotional pressure on the donor’s family; the process of organising the procedure in an emergency can increase the surgical risk for the donor. This is different in Asian countries, where the availability of cadaveric liver donors is low and where living donor LTx is undertaken on a routine basis. The results of living donor LTx in patients with ALF in Asia are good, and similar to cadaveric liver donor in Europe and USA [342]. Journal of Hepatology 2017 vol. 66 j 1047–1081 1071 Clinical Practice Guidelines Specific issues and immediate complications The context of LTx for patients with ALF is different to the elective situation; patients frequently have established extrahepatic organ failure at the time of surgery, and marginal grafts are used more frequently. The main cause of morbidity and mortality following LTx is that of sepsis, progressive organ failure in the context of vasoplegic shock, and liver graft dysfunction or failure. Cerebral deaths resultant upon cerebral oedema and herniation are now rare [8,317]. Retransplantation is more frequent than in elective series. The main causes of retransplantation are primary graft non-function and severe dysfunction, and hepatic artery thrombosis. However, outcome has also improved over time. Considerations for future studies Definition and validation of contraindications to transplant in patients with ALF. Definition and validation of futility of LTx in patients with ALF. Clarification of the role of auxiliary LTx in patients with ALF. Definition of long-term outcomes including quality of life in both transplant recipients and spontaneous survivors. Biomarkers of regenerative capacity. HBV recurrence after LTx for fulminant hepatitis B or hepatitis delta HBV recurrence can occur after transplantation for fulminant hepatitis B but is much less frequent compared to patients transplanted for chronic liver disease due to HBV. With modern antiviral agents, it should no longer occur [343]. Quality of life and long-term survival The quality of life of LTx survivors is generally good and seems similar to that of patients transplanted for chronic liver disease. The majority of young patients will return to a normal social life and to work. Psychological troubles can be observed in the early postoperative period and are explained mainly by pre-transplant HE and by the fact that these patients were not prepared psychologically for transplantation [332]. Longterm survival is generally good; there are few deaths one year post-LTx. This is due in part to the young age of the patients, the low rate of HBV recurrence in fulminant hepatitis B and the absence of recurrence of hepatic diseases, although chronic rejection remains a risk. Recommendations Assessment of patients with ALF for emergency LTx requires input from a multidisciplinary team with appropriate experience in this process (evidence level III, grade of recommendation 1). Patients with ALF, potential for deterioration and who may be candidates for LTx, should be transferred to specialist units before the onset of HE to facilitate assessment (evidence level III, grade of recommendation 1). Patients with ALF listed for LTx should be afforded the highest priority for donated organs (evidence level III, grade of recommendation 1). Irreversible brain injury is a contraindication to proceeding with LTx (evidence level II-3, grade of recommendation 1). Patients transplanted for acute HBV infection need ongoing therapy for suppression of viral replication (evidence level II-3, grade of recommendation 1). 1072 Paediatric acute liver failure ALF in children is defined as a multisystem syndrome with the following components to the definition: hepatic-based coagulopathy defined as a PT >15 s or INR >1.5 not corrected by vitamin K in the presence of clinical HE, or a PT 20 s or INR 2.0 regardless of the presence or absence of HE. An essential component of the definition is the absence of a recognised underlying chronic liver disease. A difference of note is that HE is not considered to be an essential component of the definition of ALF in children [96]. Common aetiologies Acute viral hepatitis is the most common identified cause in most of the series from Asia and South America. In contrast, in Europe and North America, aetiology remains indeterminate in about half of the patients. Patients in the indeterminate group tend to have severe disease and a high fatality rate without LTx. About 10% of these patients can develop bone marrow failure either simultaneously or a few weeks to months after the onset of symptoms of ALF [344]. Paracetamol, the most common drug associated with ALF, is safe when used in therapeutic doses in healthy children. However, inadvertent administration of higher doses of paracetamol can lead to ALF. A detailed history of exposure to paracetamol is helpful. Autoimmune hepatitis, presenting as ALF can be difficult to diagnose because some cases may not have antibody positivity at presentation. Most of these patients have a liver-kidney microsomal antibody. Children with autoimmune hepatitis presenting with ALF along with HE usually do not respond to any form of immunosuppression and need urgent LTx [345,346]. Giant cell hepatitis may also often present with autoimmune haemolytic anaemia [347]. Unknown aetiology was frequently seen in a single centre study by Kathemann et al., with better prognosis seen in older children [348]. Gestational alloimmune liver disease, earlier known as neonatal hemochromatosis (NH), is the most common cause of ALF in the neonatal period [349]. Elevation of ferritin as a diagnostic test is sensitive but not specific. Hypersaturation of transferrin with Journal of Hepatology 2017 vol. 66 j 1047–1081 JOURNAL OF HEPATOLOGY relative hypotransferrinaemia may be a valuable finding. A punch biopsy specimen of buccal minor salivary glands is a useful diagnostic tool. Documentation of iron in these minor salivary glands is highly suggestive of NH. ALF due to underlying metabolic disease is an important differential in children. A high index of suspicion is important because urgent intervention such as dietary manipulation or disease-specific treatment may be lifesaving. ALF presentation without jaundice should be an indicator to investigate underlying metabolic conditions. Mitochondrial hepatopathies should be considered if there is evidence of hypoglycaemia, vomiting, coagulopathy, acidosis and increased lactate with or without neurological symptoms. Sodium valproate is known to unmask underlying mitochondrial cytopathies [350]; hence, detailed investigations to exclude mitochondrial hepatopathies should be undertaken before injury is ascribed to sodium valproate. HLH is a common cause of ALF in children [39]. This condition presents as a spectrum of inherited and acquired conditions, with disturbed immunoregulation and coagulopathy, high fever, hepatosplenomegaly, high alkaline phosphatase, high lactate dehydrogenase, and abnormalities on peripheral blood film. Bone marrow examination or liver biopsy is diagnostic. LTx is the only proven treatment that has improved the outcome of ALF in children who fulfil poor prognostic criteria. Criteria for listing are not validated but an INR >4 and total bilirubin >300 lmol/L (17.6 mg/dl) irrespective of HE is the currently accepted criteria for listing in children because of poor survival with medical management [351,352]. Contraindications to LTx are fixed and dilated pupils, uncontrolled sepsis, and severe respiratory failure (ARDS). Relative contraindications are: accelerating inotropic requirements, infection unresponsive to treatment, history of progressive or severe neurological problems in which the ultimate neurological outcome may not be acceptable, or systemic disorders such as HLH, where LTx is not curative. Recommendations The definition of ALF in paediatrics is not dependent upon the presence of encephalopathy (evidence level II-3, grade of recommendation 1). Some aetiologies are specific to paediatric patients – notably metabolic disorders (evidence level II-3, grade of recommendation 1). Transplantation criteria are different to those in adults (evidence level II-3, grade of recommendation 1). Prognosis The prognosis of ALF varies greatly with the underlying aetiology. PT or INR is the best indicator of survival. Fulminant Wilson disease is invariably fatal, and emergency LTx is the only effective treatment. The revised Wilson disease prognostic index has been useful in identifying the patients who have a high risk of mortality without LTx [61,97]. This index incorporates bilirubin, INR, AST, white blood cell count, and albumin at presentation. A score of 11 or more indicates high mortality, with 93% sensitivity and 98% specificity with a positive predictive value of 88%. Considerations for future studies International epidemiological studies in children with ALF. Refining transplant criteria for paediatric cases. Randomised or alternative methodologies to assess best clinical practice for ALF management in children. Management A careful and detailed history should include the mode of onset of illness, family history of liver disease, consanguinity, and exposure to drugs and toxins. Clinical examination could give diagnostic clues such as the presence of any herpetic vesicles, signs of underlying chronic liver disease, and the presence of KayserFleischer rings on slit lamp examination. Specific management pertaining to paediatric disease processes can be delineated as follows: 1) Protein restriction under 1 g/kg body weight is not recommended unless the patient has an underlying urea cycle defect or organic acidaemia. 2) In neonatal liver failure, high dose intravenous acyclovir should be commenced until herpes simplex virus infection is excluded. 3) Prophylactic broad spectrum antibiotics and antifungals should be used in children admitted to high dependency or intensive care unit. 4) Use of ICP monitoring is not routinely indicated but may be considered in children older than 2 years who have clinical signs of increased ICP and are awaiting LTx. 5) Ventilatory support in the form of mechanical ventilation is instituted when grade 3 HE develops or when patients in grade 1 or 2 HE require sedation [96,351]. Conflict of interest Dr. Bernardi, Dr. Simpson, Dr. Larsen, Dr. Wendon, Dr. Manns, and Dr. Dhawan have nothing to disclose. Yaron Ilan is a consultant for Immuron, Teva, Enzo Biochem, Protalix, Therapix, Nasvax, Exalenz, Tiziana, and Natural Shield. Dr. Escorsell report other from Vital Therapies, outside the submitted work. Dr. Bernal reports personal fees from Ocera Therapeutics, personal fees from Vital Therapies, outside the submitted work. Dr. Samuel reports other from Astellas, other from BMS, other from Gilead, other from LFB, other from MSD, other from Novartis, other from Roche, other from Biotest, other from Abbvie, other from Intercept, outside the submitted work. Acknowledgements EASL would like to thank the reviewers for contributing their expertise to the production of these recommendations: Ali Canbay, François Durand and Ludwig Kramer. Journal of Hepatology 2017 vol. 66 j 1047–1081 1073 Clinical Practice Guidelines The panel would like to also acknowledge the phenomenal contribution of William Bernal, who has contributed to this work and to the management of acute liver failure. [21] [22] Supplementary data Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.jhep.2016.12. 003. [23] References [25] [1] Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924–926. [2] Andrade RJ, Lucena MI, Fernandez MC, Pelaez G, Pachkoria K, Garcia-Ruiz E, et al. Drug-induced liver injury: an analysis of 461 incidences submitted to the Spanish registry over a 10-year period. Gastroenterology 2005;129:512–521. [3] Trey C, Davidson CS. The management of fulminant hepatic failure. Prog Liver Dis 1970;3:282–398. [4] O’Grady JG, Schalm SW, Williams R. Acute liver failure: redefining the syndromes. Lancet 1993;342:273–275. [5] Bernuau J, Benhamou JP. Classifying acute liver failure. Lancet 1993;342:252–253. [6] Sugawara K, Nakayama N, Mochida S. Acute liver failure in Japan: definition, classification, and prediction of the outcome. J Gastroenterol 2012;47:849–861. [7] Tandon BN, Bernauau J, O’Grady J, Gupta SD, Krisch RE, Liaw YF, et al. Recommendations of the International Association for the Study of the Liver Subcommittee on nomenclature of acute and subacute liver failure. J Gastroenterol Hepatol 1999;14:403–404. [8] Bernal W, Hyyrylainen A, Gera A, Audimoolam VK, McPhail MJ, Auzinger G, et al. Lessons from look-back in acute liver failure? A single centre experience of 3300 patients. J Hepatol 2013;59:74–80. [9] Gimson AE, O’Grady J, Ede RJ, Portmann B, Williams R. Late onset hepatic failure: clinical, serological and histological features. Hepatology 1986;6:288–294. [10] Bernal W, Auzinger G, Dhawan A, Wendon J. Acute liver failure. Lancet 2010;376:190–201. [11] Lee WM, Stravitz RT, Larson AM. Introduction to the revised American Association for the Study of Liver Diseases Position Paper on acute liver failure 2011. Hepatology 2012;55:965–967. [12] Lee JH, Kweon OJ, Lee MK, Lee HW, Kim HJ, Kim HR. Clinical usefulness of international normalized ratio calibration of prothrombin time in patients with chronic liver disease. Int J Hematol 2015;102:163–169. [13] Duarte-Rojo A, Estradas J, Hernandez-Ramos R, Ponce-de-Leon S, Cordoba J, Torre A. Validation of the psychometric hepatic encephalopathy score (PHES) for identifying patients with minimal hepatic encephalopathy. Dig Dis Sci 2011;56:3014–3023. [14] Bernal W, Wendon J. Acute liver failure. New Engl J Med 2013;369:2525–2534. [15] Germani G, Theocharidou E, Adam R, Karam V, Wendon J, O’Grady J, et al. Liver transplantation for acute liver failure in Europe: outcomes over 20 years from the ELTR database. J Hepatol 2012;57:288–296. [16] Bernal W, Cross TJ, Auzinger G, Sizer E, Heneghan MA, Bowles M, et al. Outcome after wait-listing for emergency liver transplantation in acute liver failure: a single centre experience. J Hepatol 2009;50:306–313. [17] Ostapowicz G, Fontana RJ, Schiødt FV, Larson A, Davern TJ, Han SH, et al. Results of a prospective study of acute liver failure at 17 tertiary care centers in the United States. Ann Intern Med 2002;137:947–954. [18] Tessier G, Villeneuve E, Villeneuve JP. Etiology and outcome of acute liver failure: experience from a liver transplantation centre in Montreal. Can J Gastroenterol 2002;16:672–676. [19] Brandsaeter B, Hockerstedt K, Friman S, Ericzon BG, Kirkegaard P, Isoniemi H, et al. Fulminant hepatic failure: outcome after listing for highly urgent liver transplantation-12 years experience in the nordic countries. Liver Transpl 2002;8:1055–1162. [20] Ichai P, Legeai C, Francoz C, Boudjema K, Boillot O, Ducerf C, et al. Patients with acute liver failure listed for superurgent liver transplantation in 1074 [24] [26] [27] [28] [29] [30] [31] [32] [33] [34] [35] [36] [37] [38] [39] [40] [41] [42] [43] [44] [45] France: reevaluation of the Clichy-Villejuif criteria. Liver Transpl 2015;21:512–523. Escorsell A, Mas A, de la Mata MSpanish Group for the Study of Acute Liver Failure. Acute liver failure in Spain: analysis of 267 cases. Liver Transpl 2007;13:1389–1395. Uribe M, Buckel E, Ferrario M, Godoy J, Blanco A, Hunter B, et al. Epidemiology and results of liver transplantation for acute liver failure in Chile. Transplant Proc 2003;35:2511–2512. Gow PJ, Jones RM, Dobson JL, Angus PW. Etiology and outcome of fulminant hepatic failure managed at an Australian liver transplant unit. J Gastroenterol Hepatol 2004;19:154–159. Mudawi HM, Yousif BA. Fulminant hepatic failure in an African setting: etiology, clinical course, and predictors of mortality. Dig Dis Sci 2007;52:3266–3269. Khuroo MS, Kamili S. Aetiology and prognostic factors in acute liver failure in India. J Viral Hepat 2003;10:224–231. Hadem J, Tacke F, Bruns T, Langgartner J, Strnad P, Denk GU, et al. Etiologies and outcomes of acute liver failure in Germany. Clin Gastroenterol Hepatol 2012;10:664–669 e2. Craig DG, Bates CM, Davidson JS, Martin KG, Hayes PC, Simpson KJ. Staggered overdose pattern and delay to hospital presentation are associated with adverse outcomes following paracetamol-induced hepatotoxicity. Br J Clin Pharmacol 2012;73:285–294. Katoonizadeh A, Laleman W, Verslype C, Wilmer A, Maleux G, Roskams T, et al. Early features of acute-on-chronic alcoholic liver failure: a prospective cohort study. Gut 2010;59:1561–1569. Craig DG, Bates CM, Davidson JS, Martin KG, Hayes PC, Simpson KJ. Overdose pattern and outcome in paracetamol-induced acute severe hepatotoxicity. Br J Clin Pharmacol 2011;71:273–282. Dechene A, Sowa JP, Schlattjan M, Wree A, Blomeyer S, Best J, et al. Minilaparoscopy guided liver biopsy increases diagnostic accuracy in acute liver failure. Digestion 2014;90:240–247. Donaldson BW, Gopinath R, Wanless IR, Phillips MJ, Cameron R, Roberts EA, et al. The role of transjugular liver biopsy in fulminant liver failure: relation to other prognostic indicators. Hepatology 1993;18:1370–1376. Rich NE, Sanders C, Hughes RS, Fontana RJ, Stravitz RT, Fix O, et al. Malignant infiltration of the liver presenting as acute liver failure. Clin Gastroenterol Hepatol 2015;13:1025–1028. Rowbotham D, Wendon J, Williams R. Acute liver failure secondary to hepatic infiltration: a single centre experience of 18 cases. Gut 1998;42:576–580. Eapen CE, Velissaris D, Heydtmann M, Gunson B, Olliff S, Elias E. Favourable medium term outcome following hepatic vein recanalisation and/or transjugular intrahepatic portosystemic shunt for Budd Chiari syndrome. Gut 2006;55:878–884. Henrion J. Hypoxic hepatitis. Liver Int 2012;32:1039–1052. Fuhrmann V, Kneidinger N, Herkner H, Heinz G, Nikfardjam M, Bojic A, et al. Impact of hypoxic hepatitis on mortality in the intensive care unit. Intensive Care Med 2011;37:1302–1310. Campos Franco J, Martinez Rey C, Perez Becerra E, Gonzalez Quintela A. Cocaine related fulminant liver failure. An Med Interna 2002;19:365–367. Lange-Brock N, Berg T, Muller AR, Fliege H, Neuhaus P, Wiedenmann B, et al. Acute liver failure following the use of ecstasy (MDMA). Z Gastroenterol 2002;40:581–586. Maharaj R, Pingitore A, Menon K, Kane P, Wendon J, Bernal W. MDMAinduced acute liver failure and transient abdominal pneumatosis. Am J Gastroenterol 2015;110:963. Price B, Lines J, Lewis D, Holland N. Haemophagocytic lymphohistiocytosis: A fulminant syndrome associated with multiorgan failure and high mortality that frequently masquerades as sepsis and shock. S Afr Med J 2014;104:401–406. Anand AC, Garg HK. Approach to clinical syndrome of jaundice and encephalopathy in tropics. J Clin Exp Hepatol 2015;5:S116–S130. Larson AM, Polson J, Fontana RJ, Davern TJ, Lalani E, Hynan LS, et al. Acetaminophen-induced acute liver failure: results of a United States multicenter, prospective study. Hepatology 2005;42:1364–1372. James LP, Alonso EM, Hynan LS, Hinson JA, Davern TJ, Lee WM, et al. Detection of acetaminophen protein adducts in children with acute liver failure of indeterminate cause. Pediatrics 2006;118:e676–e681. Bernal W, Wendon J. Acute liver failure. Curr Opin Anaesthesiol 2000;13:113–118. Craig DG, Reid TW, Martin KG, Davidson JS, Hayes PC, Simpson KJ. The systemic inflammatory response syndrome and sequential organ failure assessment scores are effective triage markers following paracetamol (acetaminophen) overdose. Aliment Pharmacol Ther 2011;34:219–228. Journal of Hepatology 2017 vol. 66 j 1047–1081 JOURNAL OF HEPATOLOGY [46] Craig DG, Zafar S, Reid TW, Martin KG, Davidson JS, Hayes PC, et al. The sequential organ failure assessment (SOFA) score is an effective triage marker following staggered paracetamol (acetaminophen) overdose. Aliment Pharmacol Ther 2012;35:1408–1415. [47] Harrison PM, Keays R, Bray GP, Alexander GJ, Williams R. Improved outcome of paracetamol-induced fulminant hepatic failure by late administration of acetylcysteine. Lancet 1990;335:1572–1573. [48] Harrison PM, O’Grady JG, Keays RT, Alexander GJ, Williams R. Serial prothrombin time as prognostic indicator in paracetamol induced fulminant hepatic failure. BMJ 1990;301:964–966. [49] Keays R, Harrison PM, Wendon JA, Forbes A, Gove C, Alexander GJ, et al. Intravenous acetylcysteine in paracetamol induced fulminant hepatic failure: a prospective controlled trial. BMJ 1991;303:1026–1029. [50] McGregor AH, More LJ, Simpson KJ, Harrison DJ. Liver death and regeneration in paracetamol toxicity. Hum Exp Toxicol 2003;22:221–227. [51] Dechene A, Sowa JP, Gieseler RK, Jochum C, Bechmann LP, El Fouly A, et al. Acute liver failure is associated with elevated liver stiffness and hepatic stellate cell activation. Hepatology 2010;52:1008–1016. [52] Bechmann LP, Jochum C, Kocabayoglu P, Sowa JP, Kassalik M, Gieseler RK, et al. Cytokeratin 18-based modification of the MELD score improves prediction of spontaneous survival after acute liver injury. J Hepatol 2010;53:639–647. [53] Carrascosa MF, Salcines-Caviedes JR, Lucena MI, Andrade RJ. Acute liver failure following atorvastatin dose escalation: is there a threshold dose for idiosyncratic hepatotoxicity? J Hepatol 2015;62:751–752. [54] Lucena MI, Kaplowitz N, Hallal H, Castiella A, Garcia-Bengoechea M, Otazua P, et al. Recurrent drug-induced liver injury (DILI) with different drugs in the Spanish Registry: the dilemma of the relationship to autoimmune hepatitis. J Hepatol 2011;55:820–827. [55] Sgro C, Clinard F, Ouazir K, Chanay H, Allard C, Guilleminet C, et al. Incidence of drug-induced hepatic injuries: a French population-based study. Hepatology 2002;36:451–455. [56] Reuben A, Koch DG, Lee WM. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology 2010;52:2065–2076. [57] Roales-Gomez V, Molero AI, Perez-Amarilla I, Casabona-Frances S, ReyDiaz-Rubio E, Catalan M, et al. DRESS syndrome secondary to ibuprofen as a cause of hyperacute liver failure. Rev Esp Enferm Dig 2014;106:482–486. [58] Bosdure E, Cano A, Roquelaure B, Reynaud R, Boyer M, Viard L, et al. Oxcarbazepine and DRESS syndrome: a paediatric cause of acute liver failure. Arch Pediatr 2004;11:1073–1077. [59] Syn WK, Naisbitt DJ, Holt AP, Pirmohamed M, Mutimer DJ. Carbamazepineinduced acute liver failure as part of the DRESS syndrome. Int J Clin Pract 2005;59:988–991. [60] Kocaoglu C, Cilasun C, Solak ES, Kurtipek GS, Arslan S. Successful Treatment of antiepileptic drug-Induced DRESS syndrome with pulse methylprednisolone. Case Rep Pediatr 2013;2013:928910. [61] Devarbhavi H, Singh R, Patil M, Sheth K, Adarsh CK, Balaraju G. Outcome and determinants of mortality in 269 patients with combination antituberculosis drug-induced liver injury. J Gastroenterol Hepatol 2013;28:161–167. [62] Wai CT, Tan BH, Chan CL, Sutedja DS, Lee YM, Khor C, et al. Drug-induced liver injury at an Asian center: a prospective study. Liver Int 2007;27:465–474. [63] Ramappa V, Aithal GP. Hepatotoxicity Related to Anti-tuberculosis Drugs: Mechanisms and Management. J Clin Exp Hepatol 2013;3:37–49. [64] Hosseinnezhad A, Vijayakrishnan R, Farmer MJ. Acute renal failure, thrombocytopenia, and elevated liver enzymes after concurrent abuse of alcohol and cocaine. Clin Pract 2011;1 e35. [65] Nakamoto S, Kanda T, Nakaseko C, Sakaida E, Ohwada C, Takeuchi M, et al. Reactivation of hepatitis B virus in hematopoietic stem cell transplant recipients in Japan: efficacy of nucleos(t)ide analogues for prevention and treatment. Int J Mol Sci 2014;15:21455–21467. [66] Chang ML, Liaw YF. Hepatitis B flares in chronic hepatitis B: pathogenesis, natural course, and management. J Hepatol 2014;61:1407–1417. [67] Rantala M, van de Laar MJ. Surveillance and epidemiology of hepatitis B and C in Europe - a review. Euro Surveill 2008;13, pii=18880. [68] Bianco E, Stroffolini T, Spada E, Szklo A, Marzolini F, Ragni P, et al. Case fatality rate of acute viral hepatitis in Italy: 1995–2000. An update. Dig Liver Dis 2003;35:404–408. [69] Pande C, Sarin SK, Patra S, Bhutia K, Mishra SK, Pahuja S, et al. Prevalence, risk factors and virological profile of chronic hepatitis B virus infection in pregnant women in India. J Med Virol 2011;83:962–967. [70] Manka P, Bechmann LP, Coombes JD, Thodou V, Schlattjan M, Kahraman A, et al. Hepatitis E virus infection as a possible cause of acute liver failure in europe. Clin Gastroenterol Hepatol 2015;13:1836–1842. [71] Jochum C, Gieseler RK, Gawlista I, Fiedler A, Manka P, Saner FH, et al. Hepatitis B-associated acute liver failure: immediate treatment with entecavir inhibits hepatitis B virus replication and potentially its sequelae. Digestion 2009;80:235–240. [72] Yeo W, Ho WM, Hui P, Chan PK, Lam KC, Lee JJ, et al. Use of lamivudine to prevent hepatitis B virus reactivation during chemotherapy in breast cancer patients. Breast Cancer Res Treat 2004;88:209–215. [73] Yeo W, Zee B, Zhong S, Chan PK, Wong WL, Ho WM, et al. Comprehensive analysis of risk factors associating with Hepatitis B virus (HBV) reactivation in cancer patients undergoing cytotoxic chemotherapy. Br J Cancer 2004;90:1306–1311. [74] Seetharam A, Perrillo R, Gish R. Immunosuppression in patients with chronic hepatitis B. Curr Hepatol Rep 2014;13:235–244. [75] Wasmuth JC, Fischer HP, Sauerbruch T, Dumoulin FL. Fatal acute liver failure due to reactivation of hepatitis B following treatment with fludarabine/ cyclophosphamide/rituximab for low grade non-Hodgkin’s lymphoma. Eur J Med Res 2008;13:483–486. [76] Wai CT, Fontana RJ, Polson J, Hussain M, Shakil AO, Han SH, et al. Clinical outcome and virological characteristics of hepatitis B-related acute liver failure in the United States. J Viral Hepat 2005;12:192–198. [77] Ajmera V, Xia G, Vaughan G, Forbi JC, Ganova-Raeva LM, Khudyakov Y, et al. What factors determine the severity of hepatitis A-related acute liver failure? J Viral Hepat 2011;18:e167–e174. [78] Taylor RM, Davern T, Munoz S, Han SH, McGuire B, Larson AM, et al. Fulminant hepatitis A virus infection in the United States: Incidence, prognosis, and outcomes. Hepatology 2006;44:1589–1597. [79] Rezende G, Roque-Afonso AM, Samuel D, Gigou M, Nicand E, Ferre V, et al. Viral and clinical factors associated with the fulminant course of hepatitis A infection. Hepatology 2003;38:613–618. [80] Dalton HR, Stableforth W, Hazeldine S, Thurairajah P, Ramnarace R, Warshow U, et al. Autochthonous hepatitis E in Southwest England: a comparison with hepatitis A. Eur J Clin Microbiol Infect Dis 2008;27:579–585. [81] Mansuy JM, Abravanel F, Miedouge M, Mengelle C, Merviel C, Dubois M, et al. Acute hepatitis E in south-west France over a 5-year period. J Clin Virol 2009;44:74–77. [82] Bernuau J, Nicand E, Durand F. Hepatitis E-associated acute liver failure in pregnancy: an Indian puzzle. Hepatology 2008;48:1380–1382. [83] Shalimar, Acharya SK. Hepatitis E and acute liver failure in pregnancy. J Clin Exp Hepatol 2013;3:213–224. [84] Borkakoti J, Hazam RK, Mohammad A, Kumar A, Kar P. Does high viral load of hepatitis E virus influence the severity and prognosis of acute liver failure during pregnancy? J Med Virol 2013;85:620–626. [85] Borkakoti J, Ahmed G, Hussain SA, Rai A, Kar P. Novel molecular alterations in the ORF 2 capsid gene of hepatitis E virus in patients with acute liver failure in North India. Arch Virol 2014;159:3391–3394. [86] Levitsky J, Duddempudi AT, Lakeman FD, Whitley RJ, Luby JP, Lee WM, et al. Detection and diagnosis of herpes simplex virus infection in adults with acute liver failure. Liver Transpl 2008;14:1498–1504. [87] Ichai P, Roque Afonso AM, Sebagh M, Gonzalez ME, Codes L, Azoulay D, et al. Herpes simplex virus-associated acute liver failure: a difficult diagnosis with a poor prognosis. Liver Transpl 2005;11:1550–1555. [88] Chen M, Suzuki A, Borlak J, Andrade RJ, Lucena MI. Drug-induced liver injury: Interactions between drug properties and host factors. J Hepatology 2015;63:503–514. [89] Bernal W, Ma Y, Smith HM, Portmann B, Wendon J, Vergani D. The significance of autoantibodies and immunoglobulins in acute liver failure: a cohort study. J Hepatol 2007;47:664–670. [90] Bernal W, Meda F, Ma Y, Bogdanos DP, Vergani D. Disease-specific autoantibodies in patients with acute liver failure: the King’s College London Experience. Hepatology 2008;47:1096–1097. [91] Heneghan MA, Yeoman AD, Verma S, Smith AD, Longhi MS. Autoimmune hepatitis. Lancet 2013;382:1433–1444. [92] Karkhanis J, Verna EC, Chang MS, Stravitz RT, Schilsky M, Lee WM, et al. Steroid use in acute liver failure. Hepatology 2014;59:612–621. [93] Ichai P, Duclos-Vallee JC, Guettier C, Hamida SB, Antonini T, Delvart V, et al. Usefulness of corticosteroids for the treatment of severe and fulminant forms of autoimmune hepatitis. Liver Transpl 2007;13:996–1003. [94] James LP, Letzig L, Simpson PM, Capparelli E, Roberts DW, Hinson JA, et al. Pharmacokinetics of acetaminophen-protein adducts in adults with acetaminophen overdose and acute liver failure. Drug Metab Dispos 2009;37:1779–1784. [95] Oldakowska-Jedynak U, Ziarkiewicz M, Ziarkiewicz-Wroblewska B, Dwilewicz-Trojaczek J, Gornicka B, Nyckowski P, et al. Myeloproliferative neoplasms and recurrent thrombotic events in patients undergoing liver Journal of Hepatology 2017 vol. 66 j 1047–1081 1075 Clinical Practice Guidelines [96] [97] [98] [99] [100] [101] [102] [103] [104] [105] [106] [107] [108] [109] [110] [111] [112] [113] [114] [115] [116] [117] [118] transplantation for Budd-Chiari syndrome: a single-center experience. Ann Transplant 2014;19:591–597. Dhawan A. Acute liver failure in children and adolescents. Clin Res Hepatol Gastroenterol 2012;36:278–283. Dhawan A, Taylor RM, Cheeseman P, De Silva P, Katsiyiannakis L, MieliVergani G. Wilson’s disease in children: 37-year experience and revised King’s score for liver transplantation. Liver Transpl 2005;11:441–448. Korman JD, Volenberg I, Balko J, Webster J, Schiodt FV, Squires Jr RH, et al. Screening for Wilson disease in acute liver failure: a comparison of currently available diagnostic tests. Hepatology 2008;48:1167–1174. Loudianos G, Zappu A, Lepori MB, Dessi V, Mameli E, Orru S, et al. Acute liver failure due to Wilson’s disease with overlapping autoimmune hepatitis features: the coexistence of two diseases? J Pediatr Gastroenterol Nutr 2016;63:e23–e24. Matthews CE, Goonasekera C, Dhawan A, Deep A. Validity of pediatric index of mortality 2 (PIM2) score in pediatric acute liver failure. Crit Care 2014;18:665. Gores KM, Hamieh TS, Schmidt GA. Survival following investigational treatment of amanita mushroom poisoning: thistle or shamrock? Chest 2014;146:e126–e129. Vanooteghem S, Arts J, Decock S, Pieraerts P, Meersseman W, Verslype C, et al. Four patients with Amanita Phalloides poisoning. Acta Gastroenterol Belg 2014;77:353–356. Westbrook RH, Yeoman AD, Joshi D, Heaton ND, Quaglia A, O’Grady JG, et al. Outcomes of severe pregnancy-related liver disease: refining the role of transplantation. Am J Transplant 2010;10:2520–2526. Holt EW, Guy J, Gordon SM, Hofmann JC, Garcia-Kennedy R, Steady SL, et al. Acute liver failure caused by herpes simplex virus in a pregnant patient: is there a potential role for therapeutic plasma exchange? J Clin Apher 2013;28:426–429. Lambert G, Brichant JF, Hartstein G, Bonhomme V, Dewandre PY. Preeclampsia: an update. Acta Anaesthesiol Belg 2014;65:137–149. Paugam-Burtz C, Wendon J, Belghiti J, Mantz J. Case scenario: postoperative liver failure after liver resection in a cirrhotic patient. Anesthesiology 2012;116:705–711. Borregaard L, Lyngsoe BK, Fenger-Eriksen C, Gronbaek H, Brandsborg B. Acute liver failure following heat stroke after participating in a running event. Ugeskr Laeger 2014;176:V01130075. Jenniskens M, Langouche L, Vanwijngaerden YM, Mesotten D, Van den Berghe G. Cholestatic liver (dys)function during sepsis and other critical illnesses. Intensive Care Med 2016;42:16–27. Somasundaram A, Loganathan N, Varghese J, Shivakumar S, Jayanthi V. Does leptospirosis behave adversely in cirrhosis of the liver? Indian J Gastroenterol 2014;33:512–516. Berry PA, Bernal W, Pagliuca A, Sizer E, Salisbury JR, Wendon JA, et al. Multiple organ failure and severe bone marrow dysfunction in two 18 yearold Caucasian patients: Epstein-Barr virus and the haemophagocytic syndrome. Anaesthesia 2008;63:1249–1254. Habib M, Roberts LN, Patel RK, Wendon J, Bernal W, Arya R. Evidence of rebalanced coagulation in acute liver injury and acute liver failure as measured by thrombin generation. Liver Int 2014;34:672–678. Hugenholtz GC, Adelmeijer J, Meijers JC, Porte RJ, Stravitz RT, Lisman T. An unbalance between von Willebrand factor and ADAMTS13 in acute liver failure: implications for hemostasis and clinical outcome. Hepatology 2013;58:752–761. Lisman T, Bakhtiari K, Adelmeijer J, Meijers JC, Porte RJ, Stravitz RT. Intact thrombin generation and decreased fibrinolytic capacity in patients with acute liver injury or acute liver failure. J Thromb Haemost 2012;10:1312–1319. Bernal W. Lactate is important in determining prognosis in acute liver failure. J Hepatol 2010;53:209–210. Levy B, Gibot S, Franck P, Cravoisy A, Bollaert PE. Relation between muscle Na+K+ ATPase activity and raised lactate concentrations in septic shock: a prospective study. Lancet 2005;365:871–875. Krag M, Perner A, Wetterslev J, Wise MP, Borthwick M, Bendel S, et al. Prevalence and outcome of gastrointestinal bleeding and use of acid suppressants in acutely ill adult intensive care patients. Intensive Care Med 2015;41:833–845. Krag M, Perner A, Wetterslev J, Wise MP, Borthwick M, Bendel S, et al. Stress ulcer prophylaxis in the intensive care unit: an international survey of 97 units in 11 countries. Acta Anaesthesiol Scand 2015;59:576–585. Buckley NA, Dawson AH, Juurlink DN, Isbister GK. Who gets antidotes? Choosing the chosen few. Br J Clin Pharmacol 2016;81:402–407. 1076 [119] Harrison P, Wendon J, Williams R. Evidence of increased guanylate cyclase activation by acetylcysteine in fulminant hepatic failure. Hepatology 1996;23:1067–1072. [120] Harrison PM, Wendon JA, Gimson AE, Alexander GJ, Williams R. Improvement by acetylcysteine of hemodynamics and oxygen transport in fulminant hepatic failure. N Engl J Med 1991;324:1852–1857. [121] Lee WM, Hynan LS, Rossaro L, Fontana RJ, Stravitz RT, Larson AM, et al. Intravenous N-acetylcysteine improves transplant-free survival in early stage non-acetaminophen acute liver failure. Gastroenterology 2009;137:856–864. [122] Squires RH, Dhawan A, Alonso E, Narkewicz MR, Shneider BL, RodriguezBaez N, et al. Intravenous N-acetylcysteine in pediatric patients with nonacetaminophen acute liver failure: a placebo-controlled clinical trial. Hepatology 2013;57:1542–1549. [123] Hu J, Zhang Q, Ren X, Sun Z, Quan Q. Efficacy and safety of acetylcysteine in ‘‘non-acetaminophen” acute liver failure: A meta-analysis of prospective clinical trials. Clin Res Hepatol Gastroenterol 2015;39:594–599. [124] Yang R, Miki K, He X, Killeen ME, Fink MP. Prolonged treatment with Nacetylcystine delays liver recovery from acetaminophen hepatotoxicity. Crit Care 2009;13:R55. [125] Silva SM, Carbonel AA, Taha MO, Simoes MJ, Montero EF. Proliferative activity in ischemia/reperfusion injury in hepatectomized mice: effect of Nacetylcysteine. Transplant Proc 2012;44:2321–2325. [126] Stravitz RT, Sanyal AJ, Reisch J, Bajaj JS, Mirshahi F, Cheng J, et al. Effects of N-acetylcysteine on cytokines in non-acetaminophen acute liver failure: potential mechanism of improvement in transplant-free survival. Liver Int 2013;33:1324–1331. [127] Kim do Y, Jun JH, Lee HL, Woo KM, Ryoo HM, Kim GS, et al. N-acetylcysteine prevents LPS-induced pro-inflammatory cytokines and MMP2 production in gingival fibroblasts. Arch Pharm Res 2007;30:1283–1292. [128] Droogh JM, Smit M, Absalom AR, Ligtenberg JJ, Zijlstra JG. Transferring the critically ill patient: are we there yet? Crit Care 2015;19:62. [129] Lisman T, Caldwell SH, Burroughs AK, Northup PG, Senzolo M, Stravitz RT, et al. Hemostasis and thrombosis in patients with liver disease: the ups and downs. J Hepatol 2010;53:362–371. [130] Bernal W, Donaldson N, Wyncoll D, Wendon J. Blood lactate as an early predictor of outcome in paracetamol-induced acute liver failure: a cohort study. Lancet 2002;359:558–563. [131] Levy B, Perez P, Gibot S, Gerard A. Increased muscle-to-serum lactate gradient predicts progression towards septic shock in septic patients. Intensive Care Med 2010;36:1703–1709. [132] Levy B, Perez P, Perny J. Where does the lactate come from? A rare cause of reversible inhibition of mitochondrial respiration. Crit Care 2010;14:136. [133] Levy B, Desebbe O, Montemont C, Gibot S. Increased aerobic glycolysis through beta2 stimulation is a common mechanism involved in lactate formation during shock states. Shock 2008;30:417–421. [134] Young P, Bailey M, Beasley R, Henderson S, Mackle D, McArthur C, et al. Effect of a buffered crystalloid solution vs. saline on acute kidney injury among patients in the intensive care unit: The SPLIT randomized clinical trial. JAMA 2015;314:1701–1710. [135] Yunos NM, Bellomo R, Glassford N, Sutcliffe H, Lam Q, Bailey M. Chlorideliberal vs. chloride-restrictive intravenous fluid administration and acute kidney injury: an extended analysis. Intensive Care Med 2015;41:257–264. [136] Finfer S, Myburgh J, Bellomo R. Albumin supplementation and organ function. Crit Care Med 2007;35:987–988. [137] Finfer S, Bellomo R, Boyce N, French J, Myburgh J, Norton R, et al. A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N Engl J Med 2004;350:2247–2256. [138] Caironi P, Tognoni G, Masson S, Fumagalli R, Pesenti A, Romero M, et al. Albumin replacement in patients with severe sepsis or septic shock. N Engl J Med 2014;370:1412–1421. [139] Puskarich MA, Trzeciak S, Shapiro NI, Arnold RC, Heffner AC, Kline JA, et al. Prognostic value and agreement of achieving lactate clearance or central venous oxygen saturation goals during early sepsis resuscitation. Acad Emerg Med 2012;19:252–258. [140] Puskarich MA, Jones AE. Clearing lactate is clearly betterEllipsisbut how much? Crit Care Med 2014;42:2149–2150. [141] Monnet X, Chemla D, Osman D, Anguel N, Richard C, Pinsky MR, et al. Measuring aortic diameter improves accuracy of esophageal Doppler in assessing fluid responsiveness. Crit Care Med 2007;35:477–482. [142] Monnet X, Letierce A, Hamzaoui O, Chemla D, Anguel N, Osman D, et al. Arterial pressure allows monitoring the changes in cardiac output induced by volume expansion but not by norepinephrine. Crit Care Med 2011;39:1394–1399. Journal of Hepatology 2017 vol. 66 j 1047–1081 JOURNAL OF HEPATOLOGY [143] Monnet X, Osman D, Ridel C, Lamia B, Richard C, Teboul JL. Predicting volume responsiveness by using the end-expiratory occlusion in mechanically ventilated intensive care unit patients. Crit Care Med 2009;37:951–956. [144] Monnet X, Rienzo M, Osman D, Anguel N, Richard C, Pinsky MR, et al. Passive leg raising predicts fluid responsiveness in the critically ill. Crit Care Med 2006;34:1402–1407. [145] Legrand M, Dupuis C, Simon C, Gayat E, Mateo J, Lukaszewicz AC, et al. Association between systemic hemodynamics and septic acute kidney injury in critically ill patients: a retrospective observational study. Crit Care 2013;17:R278. [146] Mitchell KH, Carlbom D, Caldwell E, Leary PJ, Himmelfarb J, Hough CL. Volume overload: prevalence, risk factors, and functional outcome in survivors of septic shock. Ann Am Thorac Soc 2015;12:1837–1844. [147] Chen H, Wu B, Gong D, Liu Z. Fluid overload at start of continuous renal replacement therapy is associated with poorer clinical condition and outcome: a prospective observational study on the combined use of bioimpedance vector analysis and serum N-terminal pro-B-type natriuretic peptide measurement. Crit Care 2015;19:135. [148] Joshi D, Saha S, Bernal W, Heaton N, Wendon J, Auzinger G. Haemodynamic response to abdominal decompression in acute Budd-Chiari syndrome. Liver Int 2011;31:1171–1178. [149] Russell JA, Walley KR, Singer J, Gordon AC, Hebert PC, Cooper DJ, et al. Vasopressin vs. norepinephrine infusion in patients with septic shock. N Engl J Med 2008;358:877–887. [150] Gordon AC, Mason AJ, Perkins GD, Stotz M, Terblanche M, Ashby D, et al. The interaction of vasopressin and corticosteroids in septic shock: a pilot randomized controlled trial. Crit Care Med 2014;42:1325–1333. [151] Shawcross DL, Davies NA, Mookerjee RP, Hayes PC, Williams R, Lee A, et al. Worsening of cerebral hyperemia by the administration of terlipressin in acute liver failure with severe encephalopathy. Hepatology 2004;39:471–475. [152] Eefsen M, Dethloff T, Frederiksen HJ, Hauerberg J, Hansen BA, Larsen FS. Comparison of terlipressin and noradrenalin on cerebral perfusion, intracranial pressure and cerebral extracellular concentrations of lactate and pyruvate in patients with acute liver failure in need of inotropic support. J Hepatol 2007;47:381–386. [153] Leone M, Asfar P, Radermacher P, Vincent JL, Martin C. Optimizing mean arterial pressure in septic shock: a critical reappraisal of the literature. Crit Care 2015;19:101. [154] D’Aragon F, Belley-Cote EP, Meade MO, Lauzier F, Adhikari NK, Briel M, et al. Blood pressure targets for vasopressor therapy: a systematic review. Shock 2015;43:530–539. [155] Levy B, Collin S, Sennoun N, Ducrocq N, Kimmoun A, Asfar P, et al. Vascular hyporesponsiveness to vasopressors in septic shock: from bench to bedside. Intensive Care Med 2010;36:2019–2029. [156] Asfar P, Meziani F, Hamel JF, Grelon F, Megarbane B, Anguel N, et al. High vs. low blood-pressure target in patients with septic shock. N Engl J Med 2014;370:1583–1593. [157] Dunser MW, Ruokonen E, Pettila V, Ulmer H, Torgersen C, Schmittinger CA, et al. Association of arterial blood pressure and vasopressor load with septic shock mortality: a post hoc analysis of a multicenter trial. Crit Care 2009;13:R181. [158] Dunser MW, Takala J, Brunauer A, Bakker J. Re-thinking resuscitation: leaving blood pressure cosmetics behind and moving forward to permissive hypotension and a tissue perfusion-based approach. Crit Care 2013;17:326. [159] Auzinger G, Willars C, Loveridge R, Best T, Vercueil A, Prachalias A, et al. Extracorporeal membrane oxygenation for refractory hypoxemia after liver transplantation in severe hepatopulmonary syndrome: a solution with pitfalls. Liver Transpl 2014;20:1141–1144. [160] Harry R, Auzinger G, Wendon J. The effects of supraphysiological doses of corticosteroids in hypotensive liver failure. Liver Int 2003;23:71–77. [161] Harry R, Auzinger G, Wendon J. The clinical importance of adrenal insufficiency in acute hepatic dysfunction. Hepatology 2002;36:395–402. [162] Etogo-Asse FE, Vincent RP, Hughes SA, Auzinger G, Le Roux CW, Wendon J, et al. High density lipoprotein in patients with liver failure; relation to sepsis, adrenal function and outcome of illness. Liver Int 2012;32:128–136. [163] Annane D, Bellissant E. Prognostic value of cortisol response in septic shock. JAMA 2000;284:308–309. [164] Boonen E, Van den Berghe G. Cortisol metabolism in critical illness: implications for clinical care. Curr Opin Endocrinol Diabetes Obes 2014;21:185–192. [165] Boonen E, Vervenne H, Meersseman P, Andrew R, Mortier L, Declercq PE, et al. Reduced cortisol metabolism during critical illness. N Engl J Med 2013;368:1477–1488. [166] Fliers E, Bianco AC, Langouche L, Boelen A. Thyroid function in critically ill patients. Lancet Diabetes Endocrinol 2015;3:816–825. [167] Boonen E, Van den Berghe G. Endocrine responses to critical illness: novel insights and therapeutic implications. J Clin Endocrinol Metab 2014;99:1569–1582. [168] Anastasiou O, Sydor S, Sowa JP, Manka P, Katsounas A, Syn WK, et al. Higher Thyroid-Stimulating Hormone, Triiodothyronine and Thyroxine Values Are Associated with Better Outcome in Acute Liver Failure. PLoS One 2015;10 e0132189. [169] Parekh NK, Hynan LS, De Lemos J, Lee WM. Elevated troponin I levels in acute liver failure: is myocardial injury an integral part of acute liver failure? Hepatology 2007;45:1489–1495. [170] Audimooolam VK, McPhail MJ, Sherwood R, Willars C, Bernal W, Wendon JA, et al. Elevated troponin I and its prognostic significance in acute liver failure. Crit Care 2012;16:R228. [171] Malhotra A. Low-tidal-volume ventilation in the acute respiratory distress syndrome. N Engl J Med 2007;357:1113–1120. [172] Futier E, Constantin JM, Paugam-Burtz C, Pascal J, Eurin M, Neuschwander A, et al. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med 2013;369:428–437. [173] Audimoolam VK, McPhail MJ, Wendon JA, Willars C, Bernal W, Desai SR, et al. Lung injury and its prognostic significance in acute liver failure. Crit Care Med 2014;42:592–600. [174] Young D, Lamb SE, Shah S, MacKenzie I, Tunnicliffe W, Lall R, et al. Highfrequency oscillation for acute respiratory distress syndrome. N Engl J Med 2013;368:806–813. [175] Gattinoni L, Pesenti A, Carlesso E. Body position changes redistribute lung computed-tomographic density in patients with acute respiratory failure: impact and clinical fallout through the following 20 years. Intensive Care Med 2013;39:1909–1915. [176] Fuhrmann V, Madl C, Mueller C, Holzinger U, Kitzberger R, Funk GC, et al. Hepatopulmonary syndrome in patients with hypoxic hepatitis. Gastroenterology 2006;131:69–75. [177] Malbrain ML, Ameloot K, Gillebert C, Cheatham ML. Cardiopulmonary monitoring in intra-abdominal hypertension. Am Surg 2011;77:S23–S30. [178] Schutz T, Bechstein WO, Neuhaus P, Lochs H, Plauth M. Clinical practice of nutrition in acute liver failure–a European survey. Clin Nutr 2004;23:975–982. [179] Plauth M, Cabre E, Riggio O, Assis-Camilo M, Pirlich M, Kondrup J, et al. ESPEN Guidelines on enteral nutrition: Liver disease. Clin Nutr 2006;25:285–294. [180] Plauth M, Cabre E, Campillo B, Kondrup J, Marchesini G, Schutz T, et al. ESPEN Guidelines on parenteral nutrition: Hepatology. Clin Nutr 2009;28:436–444. [181] Harvey SE, Parrott F, Harrison DA, Bear DE, Segaran E, Beale R, et al. Trial of the route of early nutritional support in critically ill adults. N Engl J Med 2014;371:1673–1684. [182] Casaer MP, Mesotten D, Hermans G, Wouters PJ, Schetz M, Meyfroidt G, et al. Early vs. late parenteral nutrition in critically ill adults. N Engl J Med 2011;365:506–517. [183] Langouche L, Vander Perre S, Marques M, Boelen A, Wouters PJ, Casaer MP, et al. Impact of early nutrient restriction during critical illness on the nonthyroidal illness syndrome and its relation with outcome: a randomized, controlled clinical study. J Clin Endocrinol Metab 2013;98:1006–1013. [184] Walsh TS, Wigmore SJ, Hopton P, Richardson R, Lee A. Energy expenditure in acetaminophen-induced fulminant hepatic failure. Crit Care Med 2000;28:649–654. [185] Schneeweiss B, Pammer J, Ratheiser K, Schneider B, Madl C, Kramer L, et al. Energy metabolism in acute hepatic failure. Gastroenterology 1993;105:1515–1521. [186] Clemmesen O, Ott P, Larsen FS. Splanchnic metabolism in acute liver failure and sepsis. Curr Opin Crit Care 2004;10:152–155. [187] Gordon D, Young LR, Reddy S, Bergman C, Young JD. Incidence of Clostridium difficile infection in patients receiving high-risk antibiotics with or without a proton pump inhibitor. J Hosp Infect 2016;92:173–177. [188] Sheen CL, Dillon JF, Bateman DN, Simpson KJ, MacDonald TM. Paracetamolrelated deaths in Scotland, 1994–2000. Br J Clin Pharmacol 2002;54:430–432. [189] Moore JK, Love E, Craig DG, Hayes PC, Simpson KJ. Acute kidney injury in acute liver failure: a review. Expert Rev Gastroenterol Hepatol 2013;7:701–712. Journal of Hepatology 2017 vol. 66 j 1047–1081 1077 Clinical Practice Guidelines [190] Mesotten D, Wauters J, Van den Berghe G, Wouters PJ, Milants I, Wilmer A. The effect of strict blood glucose control on biliary sludge and cholestasis in critically ill patients. J Clin Endocrinol Metab 2009;94:2345–2352. [191] Schetz M, Vanhorebeek I, Wouters PJ, Wilmer A, Van den Berghe G. Tight blood glucose control is renoprotective in critically ill patients. J Am Soc Nephrol 2008;19:571–578. [192] Vanhorebeek I, De Vos R, Mesotten D, Wouters PJ, De Wolf-Peeters C, Van den Berghe G. Protection of hepatocyte mitochondrial ultrastructure and function by strict blood glucose control with insulin in critically ill patients. Lancet 2005;365:53–59. [193] Thiessen SE, Vanhorebeek I, Derese I, Gunst J, Van den Berghe G. FGF21 Response to Critical Illness: Effect of blood glucose control and relation with cellular stress and survival. J Clin Endocrinol Metab 2015;100: E1319–E1327. [194] Waeschle RM, Brauer A, Hilgers R, Herrmann P, Neumann P, Quintel M, et al. Hypoglycaemia and predisposing factors among clinical subgroups treated with intensive insulin therapy. Acta Anaesthesiol Scand 2014;58:223–234. [195] Kramer AH, Roberts DJ, Zygun DA. Optimal glycemic control in neurocritical care patients: a systematic review and meta-analysis. Crit Care 2012;16:R203. [196] Shawcross DL, Wendon JA. The neurological manifestations of acute liver failure. Neurochem Int 2012;60:662–671. [197] O’Riordan A, Brummell Z, Sizer E, Auzinger G, Heaton N, O’Grady JG, et al. Acute kidney injury in patients admitted to a liver intensive therapy unit with paracetamol-induced hepatotoxicity. Nephrol Dial Transplant 2011;26:3501–3508. [198] Murphy N, Auzinger G, Bernel W, Wendon J. The effect of hypertonic sodium chloride on intracranial pressure in patients with acute liver failure. Hepatology 2004;39:464–470. [199] Klinck J, McNeill L, Di Angelantonio E, Menon DK. Predictors and outcome impact of perioperative serum sodium changes in a high-risk population. Br J Anaesth 2015;114:615–622. [200] Murphy ND, Kodakat SK, Wendon JA, Jooste CA, Muiesan P, Rela M, et al. Liver and intestinal lactate metabolism in patients with acute hepatic failure undergoing liver transplantation. Crit Care Med 2001;29:2111–2118. [201] Bagshaw SM, Bellomo R, Devarajan P, Johnson C, Karvellas CJ, Kutsiogiannis DJ, et al. Review article: Renal support in critical illness. Can J Anaesth 2010;57:999–1013. [202] Funk GC, Doberer D, Fuhrmann V, Holzinger U, Kitzberger R, Kneidinger N, et al. The acidifying effect of lactate is neutralized by the alkalinizing effect of hypoalbuminemia in non-paracetamol-induced acute liver failure. J Hepatology 2006;45:387–392. [203] Schmidt LE, Dalhoff K. Serum phosphate is an early predictor of outcome in severe acetaminophen-induced hepatotoxicity. Hepatology 2002;36:659–665. [204] Bellomo R, Kellum JA, Ronco C. Defining and classifying acute renal failure: from advocacy to consensus and validation of the RIFLE criteria. Intensive Care Med 2007;33:409–413. [205] Ronco C, Kellum JA, Bellomo R, Mehta RL. Acute Dialysis Quality Initiative (ADQI). Contrib Nephrol 2013;182:1–4. [206] Bellomo R, Kellum JA, Ronco C. Acute kidney injury. Lancet 2012;380:756–766. [207] Angeli P, Ginès P, Wong F, Bernardi M, Boyer TD, Gerbes A, et al. Diagnosis and management of acute kidney injury in patients with cirrhosis: revised consensus recommendations of the International Club of Ascites. J Hepatol 2015;62:968–974. [208] Leithead JA, Ferguson JW, Bates CM, Davidson JS, Lee A, Bathgate AJ, et al. The systemic inflammatory response syndrome is predictive of renal dysfunction in patients with non-paracetamol-induced acute liver failure. Gut 2009;58:443–449. [209] Bagshaw SM, Uchino S, Kellum JA, Morimatsu H, Morgera S, Schetz M, et al. Association between renal replacement therapy in critically ill patients with severe acute kidney injury and mortality. J Crit Care 2013;28:1011–1018. [210] Slack AJ, Auzinger G, Willars C, Dew T, Musto R, Corsilli D, et al. Ammonia clearance with haemofiltration in adults with liver disease. Liver Int 2014;34:42–48. [211] Davenport A. Is there a role for continuous renal replacement therapies in patients with liver and renal failure? Kidney Int Suppl 1999;72:S62–S66. [212] Schultheiss C, Saugel B, Phillip V, Thies P, Noe S, Mayr U, et al. Continuous venovenous hemodialysis with regional citrate anticoagulation in patients with liver failure: a prospective observational study. Crit Care 2012;16: R162. 1078 [213] Slowinski T, Morgera S, Joannidis M, Henneberg T, Stocker R, Helset E, et al. Safety and efficacy of regional citrate anticoagulation in continuous venovenous hemodialysis in the presence of liver failure: the Liver Citrate Anticoagulation Threshold (L-CAT) observational study. Crit Care 2015;19:349. [214] Patel S, Wendon J. Regional citrate anticoagulation in patients with liver failure–time for a rethink? Crit Care 2012;16:153. [215] von Mach MA, Hermanns-Clausen M, Koch I, Hengstler JG, Lauterbach M, Kaes J, et al. Experiences of a poison center network with renal insufficiency in acetaminophen overdose: an analysis of 17 cases. Clin Toxicol 2005;43:31–37. [216] Stravitz RT, Lisman T, Luketic VA, Sterling RK, Puri P, Fuchs M, et al. Minimal effects of acute liver injury/acute liver failure on hemostasis as assessed by thromboelastography. J Hepatol 2012;56:129–136. [217] Agarwal B, Gatt A, Riddell A, Wright G, Chowdary P, Jalan R, et al. Hemostasis in patients with acute kidney injury secondary to acute liver failure. Kidney Int 2013;84:158–163. [218] Stravitz RT, Bowling R, Bradford RL, Key NS, Glover S, Thacker LR, et al. Role of procoagulant microparticles in mediating complications and outcome of acute liver injury/acute liver failure. Hepatology 2013;58:304–313. [219] Munoz SJ, Rajender Reddy K, Lee WAcute Liver Failure Study Group. The coagulopathy of acute liver failure and implications for intracranial pressure monitoring. Neurocrit Care 2008;9:103–107. [220] Vaquero J, Fontana RJ, Larson AM, Bass NM, Davern TJ, Shakil AO, et al. Complications and use of intracranial pressure monitoring in patients with acute liver failure and severe encephalopathy. Liver Transpl 2005;11:1581–1589. [221] Karvellas CJ, Fix OK, Battenhouse H, Durkalski V, Sanders C, Lee WM. Outcomes and complications of intracranial pressure monitoring in acute liver failure: A retrospective cohort study. Crit Care Med 2014;42:1157–1167. [222] Kozek-Langenecker SA, Afshari A, Albaladejo P, Santullano CA, De Robertis E, Filipescu DC, et al. Management of severe perioperative bleeding: guidelines from the European Society of Anaesthesiology. Eur J Anaesthesiol 2013;30:270–382. [223] Lelubre C, Vincent JL, Taccone FS. Red blood cell transfusion strategies in critically ill patients: lessons from recent randomized clinical studies. Minerva Anestesiol 2016;82:1010–1016. [224] Rolando N, Philpott-Howard J, Williams R. Bacterial and fungal infection in acute liver failure. Semin Liver Dis 1996;16:389–402. [225] Rolando N, Harvey F, Brahm J, Philpott-Howard J, Alexander G, Casewell M, et al. Fungal infection: a common, unrecognised complication of acute liver failure. J Hepatol 1991;12:1–9. [226] Vaquero J, Polson J, Chung C, Helenowski I, Schiodt FV, Reisch J, et al. Infection and the progression of hepatic encephalopathy in acute liver failure. Gastroenterology 2003;125:755–764. [227] Karvellas CJ, Pink F, McPhail M, Cross T, Auzinger G, Bernal W, et al. Predictors of bacteraemia and mortality in patients with acute liver failure. Intensive Care Med 2009;35:1390–1396. [228] Antoniades CG, Berry PA, Wendon JA, Vergani D. The importance of immune dysfunction in determining outcome in acute liver failure. J Hepatol 2008;49:845–861. [229] Taylor NJ, Nishtala A, Manakkat Vijay GK, Abeles RD, Auzinger G, Bernal W, et al. Circulating neutrophil dysfunction in acute liver failure. Hepatology 2013;57:1142–1152. [230] Craig DG, Kitto L, Zafar S, Reid TW, Martin KG, Davidson JS, et al. An elevated neutrophil-lymphocyte ratio is associated with adverse outcomes following single time-point paracetamol (acetaminophen) overdose: a time-course analysis. Eur J Gastroenterol Hepatol 2014;26:1022–1029. [231] Lopez Roa P, Hill JA, Kirby KA, Leisenring WM, Huang ML, Santo TK, et al. Coreactivation of Human Herpesvirus 6 and Cytomegalovirus Is Associated With Worse Clinical Outcome in Critically Ill Adults. Crit Care Med 2015;43:1415–1422. [232] Limaye AP, Kirby KA, Rubenfeld GD, Leisenring WM, Bulger EM, Neff MJ, et al. Cytomegalovirus reactivation in critically ill immunocompetent patients. JAMA 2008;300:413–422. [233] Rule JA, Hynan LS, Attar N, Sanders C, Korzun WJ, Lee WM, et al. Procalcitonin identifies cell injury, not bacterial infection, in acute liver failure. PLoS One 2015;10 e0138566. [234] Silvestre JP, Coelho LM, Povoa PM. Impact of fulminant hepatic failure in Creactive protein? J Crit Care 2010;25:e7–e12. [235] Farmakiotis D, Kontoyiannis DP. Emerging issues with diagnosis and management of fungal infections in solid organ transplant recipients. Am J Transplant 2015;15:1141–1147. Journal of Hepatology 2017 vol. 66 j 1047–1081 JOURNAL OF HEPATOLOGY [236] Karvellas CJ, Cavazos J, Battenhouse H, Durkalski V, Balko J, Sanders C, et al. Effects of antimicrobial prophylaxis and blood stream infections in patients with acute liver failure: a retrospective cohort study. Clinical Gastroenterol Hepatolol 2014;12:1942–11949. [237] Rolando N, Gimson A, Wade J, Philpott-Howard J, Casewell M, Williams R. Prospective controlled trial of selective parenteral and enteral antimicrobial regimen in fulminant liver failure. Hepatology 1993;17:196–201. [238] Rolando N, Wade J, Davalos M, Wendon J, Philpott-Howard J, Williams R. The systemic inflammatory response syndrome in acute liver failure. Hepatology 2000;32:734–739. [239] Simpson KJ, Lukacs NW, McGregor AH, Harrison DJ, Strieter RM, Kunkel SL. Inhibition of tumour necrosis factor alpha does not prevent experimental paracetamol-induced hepatic necrosis. J Pathol 2000;190:489–494. [240] Bernal W, Donaldson P, Underhill J, Wendon J, Williams R. Tumor necrosis factor genomic polymorphism and outcome of acetaminophen (paracetamol)-induced acute liver failure. J Hepatol 1998;29:53–59. [241] Antoniades CG, Berry PA, Davies ET, Hussain M, Bernal W, Vergani D, et al. Reduced monocyte HLA-DR expression: a novel biomarker of disease severity and outcome in acetaminophen-induced acute liver failure. Hepatology 2006;44:34–43. [242] Berry PA, Antoniades CG, Hussain MJ, McPhail MJ, Bernal W, Vergani D, et al. Admission levels and early changes in serum interleukin-10 are predictive of poor outcome in acute liver failure and decompensated cirrhosis. Liver Int 2010;30:733–740. [243] Possamai LA, Antoniades CG, Anstee QM, Quaglia A, Vergani D, Thursz M, et al. Role of monocytes and macrophages in experimental and human acute liver failure. World J Gastroenterol 2010;16:1811–1819. [244] Craig DG, Lee P, Pryde EA, Walker SW, Beckett GJ, Hayes PC, et al. Elevated levels of the long pentraxin 3 in paracetamol-induced human acute liver injury. Eur J Gastroenterol Hepatol 2013;25:359–367. [245] Craig DG, Lee P, Pryde EA, Hayes PC, Simpson KJ. Serum neopterin and soluble CD163 as markers of macrophage activation in paracetamol (acetaminophen)-induced human acute liver injury. Aliment Pharmacol Ther 2013;38:1395–1404. [246] Antoine DJ, Jenkins RE, Dear JW, Williams DP, McGill MR, Sharpe MR, et al. Molecular forms of HMGB1 and keratin-18 as mechanistic biomarkers for mode of cell death and prognosis during clinical acetaminophen hepatotoxicity. J Hepatol 2012;56:1070–1079. [247] Abeles RD, McPhail MJ, Sowter D, Antoniades CG, Vergis N, Vijay GK, et al. CD14, CD16 and HLA-DR reliably identifies human monocytes and their subsets in the context of pathologically reduced HLA-DR expression by CD14(hi) /CD16(neg) monocytes: Expansion of CD14(hi) /CD16(pos) and contraction of CD14(lo) /CD16(pos) monocytes in acute liver failure. Cytometry A 2012;81:823–834. [248] Craig DG, Lee P, Pryde EA, Masterton GS, Hayes PC, Simpson KJ. Circulating apoptotic and necrotic cell death markers in patients with acute liver injury. Liver Int 2011;31:1127–1136. [249] Possamai LA, McPhail MJ, Quaglia A, Zingarelli V, Abeles RD, Tidswell R, et al. Character and temporal evolution of apoptosis in acetaminopheninduced acute liver failure. Crit Care Med 2013;41:2543–2550. [250] Possamai LA, Khamri W, Triantafyllou E, Wendon JA, Thursz MR, Antoniades CG. Could targeting secretory leukocyte protease inhibitor be an effective therapeutic option to prevent infections in acute liver failure? Immunotherapy 2014;6:667–669. [251] Antoniades CG, Khamri W, Abeles RD, Taams LS, Triantafyllou E, Possamai LA, et al. Secretory leukocyte protease inhibitor: a pivotal mediator of antiinflammatory responses in acetaminophen-induced acute liver failure. Hepatology 2014;59:1564–1576. [252] Antoniades CG, Quaglia A, Taams LS, Mitry RR, Hussain M, Abeles R, et al. Source and characterization of hepatic macrophages in acetaminopheninduced acute liver failure in humans. Hepatology 2012;56:735–746. [253] Schmidt LE, Larsen FS. Prognostic implications of hyperlactatemia, multiple organ failure, and systemic inflammatory response syndrome in patients with acetaminophen-induced acute liver failure. Crit Care Med 2006;34:337–343. [254] Craig DG, Reid TW, Wright EC, Martin KG, Davidson JS, Hayes PC, et al. The sequential organ failure assessment (SOFA) score is prognostically superior to the model for end-stage liver disease (MELD) and MELD variants following paracetamol (acetaminophen) overdose. Aliment Pharmacol Ther 2012;35:705–713. [255] Butterworth RF. Pathogenesis of hepatic encephalopathy and brain edema in acute liver failure. J Clin Exp Hepatol 2015;5:S96–S103. [256] Larsen FS, Wendon J. Prevention and management of brain edema in patients with acute liver failure. Liver Transpl 2008;14:S90–S96. [257] Bjerring PN, Eefsen M, Hansen BA, Larsen FS. The brain in acute liver failure. A tortuous path from hyperammonemia to cerebral edema. Metab Brain Dis 2009;24:5–14. [258] Wright G, Shawcross D, Olde Damink SW, Jalan R. Brain cytokine flux in acute liver failure and its relationship with intracranial hypertension. Metab Brain Dis 2007;22:375–388. [259] Bernal W, Hall C, Karvellas CJ, Auzinger G, Sizer E, Wendon J. Arterial ammonia and clinical risk factors for encephalopathy and intracranial hypertension in acute liver failure. Hepatology 2007;46:1844–1852. [260] Chastre A, Belanger M, Beauchesne E, Nguyen BN, Desjardins P, Butterworth RF. Inflammatory cascades driven by tumor necrosis factor-alpha play a major role in the progression of acute liver failure and its neurological complications. PLoS One 2012;7 e49670. [261] Bjerring PN, Dale N, Larsen FS. Acute hyperammonemia and systemic inflammation is associated with increased extracellular brain adenosine in rats: a biosensor study. Neurochem Res 2015;40:258–264. [262] Rohde J, Pedersen HR, Bjerring PN, Larsen FS. Effects of dexamethasone and cox inhibitors on intracranial pressure and cerebral perfusion in the lipopolysaccharide treated rats with hyperammonemia. PLoS One 2015;10 e0117416. [263] Craig DG, Ford AC, Hayes PC, Simpson KJ. Systematic review: prognostic tests of paracetamol-induced acute liver failure. Aliment Pharmacol Ther 2010;31:1064–1076. [264] Schiodt FV, Rossaro L, Stravitz RT, Shakil AO, Chung RT, Lee WM. Gcglobulin and prognosis in acute liver failure. Liver Transpl 2005;11:1223–1227. [265] Antoniades CG, Berry PA, Bruce M, Cross TJ, Portal AJ, Hussain MJ, et al. Actin-free Gc globulin: a rapidly assessed biomarker of organ dysfunction in acute liver failure and cirrhosis. Liver Transpl 2007;13:1254–1261. [266] Volkmann X, Anstaett M, Hadem J, Stiefel P, Bahr MJ, Lehner F, et al. Caspase activation is associated with spontaneous recovery from acute liver failure. Hepatology 2008;47:1624–1633. [267] Rutherford A, King LY, Hynan LS, Vedvyas C, Lin W, Lee WM, et al. Development of an accurate index for predicting outcomes of patients with acute liver failure. Gastroenterology 2012;143:1237–1243. [268] Craig DG, Simpson KJ. Accuracy of the ALFSG index as a triage marker in acute liver failure. Gastroenterology 2013;144 e25. [269] Bernsmeier C, Antoniades CG, Wendon J. What’s new in acute liver failure? Intensive Care Med 2014;40:1545–1548. [270] Larsen FS, Wendon J. Alternative pathway therapy for hyperammonemia in liver failure. Hepatology 2009;50:3–5. [271] Raghavan M, Marik PE. Therapy of intracranial hypertension in patients with fulminant hepatic failure. Neurocrit Care 2006;4:179–189. [272] Bhatia V, Batra Y, Acharya SK. Prophylactic phenytoin does not improve cerebral edema or survival in acute liver failure–a controlled clinical trial. J Hepatol 2004;41:89–96. [273] Clemmesen JO, Larsen FS, Kondrup J, Hansen BA, Ott P. Cerebral herniation in patients with acute liver failure is correlated with arterial ammonia concentration. Hepatology 1999;29:648–653. [274] Bhatia V, Singh R, Acharya SK. Predictive value of arterial ammonia for complications and outcome in acute liver failure. Gut 2006;55:98–104. [275] Tofteng F, Hauerberg J, Hansen BA, Pedersen CB, Jorgensen L, Larsen FS. Persistent arterial hyperammonemia increases the concentration of glutamine and alanine in the brain and correlates with intracranial pressure in patients with fulminant hepatic failure. J Cereb Blood Flow Metab 2006;26:21–27. [276] Karvellas CJ, Fix OK, Battenhouse H, Durkalski V, Sanders C, Lee WM, et al. Outcomes and complications of intracranial pressure monitoring in acute liver failure: a retrospective cohort study. Crit Care Med 2014;42:1157–1167. [277] Blei AT, Olafsson S, Webster S, Levy R. Complications of intracranial pressure monitoring in fulminant hepatic failure. Lancet 1993;341:157–158. [278] Wendon JA, Larsen FS. Intracranial pressure monitoring in acute liver failure. A procedure with clear indications. Hepatology 2006;44:504–506. [279] Bernuau J, Durand F. Intracranial pressure monitoring in patients with acute liver failure: a questionable invasive surveillance. Hepatology 2006;44:502–504. [280] Fortea JI, Banares R, Vaquero J. Intracranial pressure in acute liver failure: to bolt or not to bolt-that is the question. Crit Care Med 2014;42:1304–1305. [281] Larsen FS, Strauss G, Moller K, Hansen BA. Regional cerebral blood flow autoregulation in patients with fulminant hepatic failure. Liver Transpl 2000;6:795–800. [282] Krishnamoorthy V, Beckmann K, Mueller M, Sharma D, Vavilala MS. Perioperative estimation of the intracranial pressure using the optic nerve Journal of Hepatology 2017 vol. 66 j 1047–1081 1079 Clinical Practice Guidelines [283] [284] [285] [286] [287] [288] [289] [290] [291] [292] [293] [294] [295] [296] [297] [298] [299] [300] [301] [302] [303] [304] 1080 sheath diameter during liver transplantation. Liver Transpl 2013;19:246–249. Helbok R, Olson DM, Le Roux PD, Vespa PParticipants in the International Multidisciplinary Consensus Conference on Multimodality Monitoring. Intracranial pressure and cerebral perfusion pressure monitoring in nonTBI patients: special considerations. Neurocrit Care 2014;21:S85–S94. Davies MH, Mutimer D, Lowes J, Elias E, Neuberger J. Recovery despite impaired cerebral perfusion in fulminant hepatic failure. Lancet 1994;343:1329–1330. Canalese J, Gimson AE, Davis C, Mellon PJ, Davis M, Williams R. Controlled trial of dexamethasone and mannitol for the cerebral oedema of fulminant hepatic failure. Gut 1982;23:625–629. Tofteng F, Larsen FS. The effect of indomethacin on intracranial pressure, cerebral perfusion and extracellular lactate and glutamate concentrations in patients with fulminant hepatic failure. J Cereb Blood Flow Metab 2004;24:798–804. Acharya SK, Bhatia V, Sreenivas V, Khanal S, Panda SK. Efficacy of Lornithine L-aspartate in acute liver failure: a double-blind, randomized, placebo-controlled study. Gastroenterology 2009;136:2159–2168. Jalan R, Olde Damink SW, Deutz NE, Hayes PC, Lee A. Restoration of cerebral blood flow autoregulation and reactivity to carbon dioxide in acute liver failure by moderate hypothermia. Hepatology 2001;34:50–54. Jalan R, O Damink SW, Deutz NE, Lee A, Hayes PC. Moderate hypothermia for uncontrolled intracranial hypertension in acute liver failure. Lancet 1999;354:1164–1168. Nielsen N, Wetterslev J, Cronberg T, Erlinge D, Gasche Y, Hassager C, et al. Targeted temperature management at 33 degrees C vs. 36 degrees C after cardiac arrest. N Engl J Med 2013;369:2197–2206. Ringe B, Pichlmayr R, Lubbe N, Bornscheuer A, Kuse E. Total hepatectomy as temporary approach to acute hepatic or primary graft failure. Transplant Proc 1988;20:552–557. O’Grady JG, Gimson AE, O’Brien CJ, Pucknell A, Hughes RD, Williams R. Controlled trials of charcoal hemoperfusion and prognostic factors in fulminant hepatic failure. Gastroenterology 1988;94:1186–1192. Gimson AE, Braude S, Mellon PJ, Canalese J, Williams R. Earlier charcoal haemoperfusion in fulminant hepatic failure. Lancet 1982;2:681–683. Karvellas CJ, Gibney N, Kutsogiannis D, Wendon J, Bain VG. Bench-tobedside review: current evidence for extracorporeal albumin dialysis systems in liver failure. Crit Care 2007;11:215. Lai WK, Haydon G, Mutimer D, Murphy N. The effect of molecular adsorbent recirculating system on pathophysiological parameters in patients with acute liver failure. Intensive Care Med 2005;31:1544–1549. Schmidt LE, Wang LP, Hansen BA, Larsen FS. Systemic hemodynamic effects of treatment with the molecular adsorbents recirculating system in patients with hyperacute liver failure: a prospective controlled trial. Liver Transpl 2003;9:290–297. Kantola T, Koivusalo AM, Hockerstedt K, Isoniemi H. The effect of molecular adsorbent recirculating system treatment on survival, native liver recovery, and need for liver transplantation in acute liver failure patients. Transpl Int 2008;21:857–866. Kribben A, Gerken G, Haag S, Herget-Rosenthal S, Treichel U, Betz C, et al. Effects of fractionated plasma separation and adsorption on survival in patients with acute-on-chronic liver failure. Gastroenterology 2012;142:782–789. Evenepoel P, Laleman W, Wilmer A, Claes K, Kuypers D, Bammens B, et al. Prometheus vs. molecular adsorbents recirculating system: comparison of efficiency in two different liver detoxification devices. Artif Organs 2006;30:276–284. Tsipotis E, Shuja A, Jaber BL. Albumin dialysis for liver failure: a systematic review. Adv Chronic Kidney Dis 2015;22:382–390. Stutchfield BM, Simpson K, Wigmore SJ. Systematic review and metaanalysis of survival following extracorporeal liver support. Br J Surg 2011;98:623–631. Saliba F, Camus C, Durand F, Mathurin P, Letierce A, Delafosse B, et al. Albumin dialysis with a noncell artificial liver support device in patients with acute liver failure: a randomized, controlled trial. Ann Int Med 2013;159:522–531. Samuel D, Ichai P, Feray C, Saliba F, Azoulay D, Arulnaden JL, et al. Neurological improvement during bioartificial liver sessions in patients with acute liver failure awaiting transplantation. Transplantation 2002;73:257–264. Demetriou AA, Brown Jr RS, Busuttil RW, Fair J, McGuire BM, Rosenthal P, et al. Prospective, randomized, multicenter, controlled trial of a bioartificial liver in treating acute liver failure. Ann Surg 2004;239:660–667. [305] Miwa Y, Ellis AJ, Hughes RD, Langley PG, Wendon JA, Williams R. Effect of ELAD liver support on plasma HGF and TGF-beta 1 in acute liver failure. Int J Artif Organs 1996;19:240–244. [306] Ibars EP, Cortes M, Tolosa L, Gomez-Lechon MJ, Lopez S, Castell JV, et al. Hepatocyte transplantation program: Lessons learned and future strategies. World J Gastroenterol 2016;22:874–886. [307] Legido-Quigley C, Cloarec O, Parker DA, Murphy GM, Holmes E, Lindon JC, et al. First example of hepatocyte transplantation to alleviate ornithine transcarbamylase deficiency, monitored by NMR-based metabonomics. Bioanalysis 2009;1:1527–1535. [308] Clemmesen JO, Kondrup J, Nielsen LB, Larsen FS, Ott P. Effects of highvolume plasmapheresis on ammonia, urea, and amino acids in patients with acute liver failure. Am J Gastroenterol 2001;96:1217–1223. [309] Clemmesen JO, Gerbes AL, Gulberg V, Hansen BA, Larsen FS, Skak C, et al. Hepatic blood flow and splanchnic oxygen consumption in patients with liver failure. Effect of high-volume plasmapheresis. Hepatology 1999;29:347–355. [310] Larsen FS, Schmidt LE, Bernsmeier C, Rasmussen A, Isoniemi H, Patel VC, et al. High-volume plasma exchange in patients with acute liver failure: An open randomised controlled trial. J Hepatol 2016;64:69–78. [311] Morelli A, Ertmer C, Westphal M, Rehberg S, Kampmeier T, Ligges S, et al. Effect of heart rate control with esmolol on hemodynamic and clinical outcomes in patients with septic shock: a randomized clinical trial. JAMA 2013;310:1683–1691. [312] Kramer L, Bauer E, Gendo A, Madl C, Gangl A. Influence of hydroxy ethyl starch infusion on serum bilirubin levels in cirrhotic patients treated with artificial liver support. Int J Artif Organs 2002;25:918–922. [313] Personett HA, Larson SL, Frazee EN, Nyberg SL, El-Zoghby ZM. Extracorporeal elimination of Piperacillin/Tazobactam during molecular adsorbent recirculating system therapy. Pharmacotherapy 2015;35:e136–e319. [314] Personett HA, Larson SL, Frazee EN, Nyberg SL, Leung N, El-Zoghby ZM. Impact of molecular adsorbent recirculating system therapy on tacrolimus elimination: a case report. Transpl Proc 2014;46:2440–2442. [315] Faybik P, Hetz H, Mitterer G, Krenn CG, Schiefer J, Funk GC, et al. Regional citrate anticoagulation in patients with liver failure supported by a molecular adsorbent recirculating system. Crit Care Med 2011;39:273–279. [316] Langley PG, Keays R, Hughes RD, Forbes A, Delvos U, Williams R. Antithrombin III supplementation reduces heparin requirement and platelet loss during hemodialysis of patients with fulminant hepatic failure. Hepatology 1991;14:251–256. [317] Neuberger J, Gimson A, Davies M, Akyol M, O’Grady J, Burroughs A, et al. Selection of patients for liver transplantation and allocation of donated livers in the UK. Gut 2008;57:252–257. [318] Bernuau J, Goudeau A, Poynard T, Dubois F, Lesage G, Yvonnet B, et al. Multivariate analysis of prognostic factors in fulminant hepatitis B. Hepatology 1986;6:648–651. [319] Pereira LM, Langley PG, Hayllar KM, Tredger JM, Williams R. Coagulation factor V and VIII/V ratio as predictors of outcome in paracetamol induced fulminant hepatic failure: relation to other prognostic indicators. Gut 1992;33:98–102. [320] Izumi S, Langley PG, Wendon J, Ellis AJ, Pernambuco RB, Hughes RD, et al. Coagulation factor V levels as a prognostic indicator in fulminant hepatic failure. Hepatology 1996;23:1507–1511. [321] O’Grady JG, Alexander GJ, Hayllar KM, Williams R. Early indicators of prognosis in fulminant hepatic failure. Gastroenterology 1989;97:439–445. [322] Hadem J, Stiefel P, Bahr MJ, Tillmann HL, Rifai K, Klempnauer J, et al. Prognostic implications of lactate, bilirubin, and etiology in German patients with acute liver failure. Clin Gastroenterol Hepatol 2008;6:339–345. [323] Bernuau J, Samuel D, Durand F, et al. Criteria for emergency liver transplantation in patients with acute viral hepatitis and factor V below 50% of normal: a prospective study. Hepatology 1991;14:49A. [324] McPhail MJ, Farne H, Senvar N, Wendon JA, Bernal W. Ability of King’s College Criteria and Model for End-Stage Liver Disease scores to predict mortality of patients with acute liver failure: A meta-analysis. Clin Gastroenterol Hepatol 2016;14:516–525. [325] McPhail MJ, Wendon JA, Bernal W. Meta-analysis of performance of Kings’s College Hospital Criteria in prediction of outcome in non-paracetamolinduced acute liver failure. J Hepatol 2010;53:492–499. [326] Schmidt LE, Ott P, Tygstrup N. Galactose elimination capacity as a prognostic marker in patients with severe acetaminophen-induced hepatotoxicity: 10 years’ experience. Clin Gastroenterol Hepatol 2004;2:418–424. Journal of Hepatology 2017 vol. 66 j 1047–1081 JOURNAL OF HEPATOLOGY [327] Hendrichova M, Malek F, Koprivova H, Vranova J, Ostadal P, Kratka K, et al. Correlation of NT-proBNP with metabolic liver function as assessed with (13)C-methacetin breath test in patients with acute decompensated heart failure. Int J Cardiol 2010;144:321–322. [328] Feng HL, Li Q, Wang L, Yuan GY, Cao WK. Indocyanine green clearance test combined with MELD score in predicting the short-term prognosis of patients with acute liver failure. Hepatobiliary Pancreat Dis Int 2014;13:271–275. [329] Halle BM, Poulsen TD, Pedersen HP. Indocyanine green plasma disappearance rate as dynamic liver function test in critically ill patients. Acta Anaesthesiol Scand 2014;58:1214–1219. [330] Quintero J, Miserachs M, Ortega J, Bueno J, Dopazo C, Bilbao I, et al. Indocyanine green plasma disappearance rate: a new tool for the classification of paediatric patients with acute liver failure. Liver Int 2014;34:689–694. [331] Merle U, Sieg O, Stremmel W, Encke J, Eisenbach C. Sensitivity and specificity of plasma disappearance rate of indocyanine green as a prognostic indicator in acute liver failure. BMC Gastroenterol 2009;9:91. [332] Karvellas CJ, Safinia N, Auzinger G, Heaton N, Muiesan P, O’Grady J, et al. Medical and psychiatric outcomes for patients transplanted for acetaminophen-induced acute liver failure: a case-control study. Liver Int 2010;30:826–833. [333] Shukla A, Vadeyar H, Rela M, Shah S. Liver transplantation: east vs. west. J Clin Exp Hepatol 2013;3:243–253. [334] Gurevich M, Guy-Viterbo V, Janssen M, Stephenne X, Smets F, Sokal E, et al. Living donor liver transplantation in children: surgical and immunological results in 250 recipients at Universite Catholique de Louvain. Ann Surg 2015;262:1141–1149. [335] Lee J, Lee JG, Lee JJ, Kim MS, Ju MK, Choi GH, et al. Results of ABOincompatible liver transplantation using a simplified protocol at a single institution. Transpl Proc 2015;47:723–726. [336] Wigg AJ, Gunson BK, Mutimer DJ. Outcomes following liver transplantation for seronegative acute liver failure: experience during a 12-year period with more than 100 patients. Liver Transpl 2005;11:27–34. [337] Cooper SC, Aldridge RC, Shah T, Webb K, Nightingale P, Paris S, et al. Outcomes of liver transplantation for paracetamol (acetaminophen)induced hepatic failure. Liver Transpl 2009;15:1351–1357. [338] Rajput I, Prasad KR, Bellamy MC, Davies M, Attia MS, Lodge JP. Subtotal hepatectomy and whole graft auxiliary transplantation for acetaminophenassociated acute liver failure. HPB 2014;16:220–228. [339] Girlanda R, Vilca-Melendez H, Srinivasan P, Muiesan P, O’Grady JG, Rela M, et al. Immunosuppression withdrawal after auxiliary liver transplantation for acute liver failure. Transpl Proc 2005;37:1720–1721. [340] Quaglia A, Portmann BC, Knisely AS, Srinivasan P, Muiesan P, Wendon J, et al. Auxiliary transplantation for acute liver failure: Histopathological study of native liver regeneration. Liver Transpl 2008;14:1437–1448. [341] Salehi S, Brereton HC, Arno MJ, Darling D, Quaglia A, O’Grady J, et al. Human liver regeneration is characterized by the coordinated expression of distinct microRNA governing cell cycle fate. Am J Transplant 2013;13:1282–1295. [342] Park SJ, Lim YS, Hwang S, Heo NY, Lee HC, Suh DJ, et al. Emergency adult-toadult living-donor liver transplantation for acute liver failure in a hepatitis B virus endemic area. Hepatology 2010;51:903–911. [343] Dao DY, Seremba E, Ajmera V, Sanders C, Hynan LS, Lee WM, et al. Use of nucleoside (tide) analogues in patients with hepatitis B-related acute liver failure. Dig Dis Sci 2012;57:1349–1357. [344] Tung J, Hadzic N, Layton M, Baker AJ, Dhawan A, Rela M, et al. Bone marrow failure in children with acute liver failure. J Pediatr Gastroenterol Nutr 2000;31:557–561. [345] Wang Q, Yang F, Miao Q, Krawitt EL, Gershwin ME, Ma X. The clinical phenotypes of autoimmune hepatitis: A comprehensive review. J Autoimmun 2016;66:98–107. [346] Longhi MS, Mieli-Vergani G, Vergani D. Autoimmune hepatitis. Curr. Pediatr Rev 2014;10:268–274. [347] Maggiore G, Sciveres M, Fabre M, Gori L, Pacifico L, Resti M, et al. Giant cell hepatitis with autoimmune hemolytic anemia in early childhood: longterm outcome in 16 children. J Pediatr 2011;159:127–132 e1. [348] Kathemann S, Bechmann LP, Sowa JP, Manka P, Dechene A, Gerner P, et al. Etiology, outcome and prognostic factors of childhood acute liver failure in a German Single Center. Ann Hepatol 2015;14:722–728. [349] Lopriore E, Mearin ML, Oepkes D, Devlieger R, Whitington PF. Neonatal hemochromatosis: management, outcome, and prevention. Prenat Diagn 2013;33:1221–1225. [350] Hynynen J, Komulainen T, Tukiainen E, Nordin A, Arola J, Kalviainen R, et al. Acute liver failure after valproate exposure in patients with POLG1 mutations and the prognosis after liver transplantation. Liver Transpl 2014;20:1402–1412. [351] Dhawan A. Etiology and prognosis of acute liver failure in children. Liver Transpl 2008;14:S80–S84. [352] Sundaram V, Shneider BL, Dhawan A, Ng VL, Im K, Belle S, et al. King’s College Hospital Criteria for non-acetaminophen induced acute liver failure in an international cohort of children. J Pediatr 2013;162:319–323 e1. Journal of Hepatology 2017 vol. 66 j 1047–1081 1081