Uploaded by
dmasyithahd
Interferon-γ and Systemic Autoimmunity: Role in Lupus and Autoimmunity
advertisement

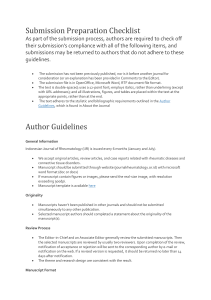
NIH Public Access Author Manuscript Discov Med. Author manuscript; available in PMC 2014 September 01. NIH-PA Author Manuscript Published in final edited form as: Discov Med. 2013 September ; 16(87): 123–131. Interferon-γ and Systemic Autoimmunity K.M. Pollarda, D.M. Cauvib, C.B Toomeyc, K.V. Morrisa,d, and D.H. Konoe aDepartment of Molecular and Experimental Medicine, The Scripps Research Institute, La Jolla, CA 92037, USA bDepartment of Surgery and Center for Investigations of Health and Education Disparities, University of California San Diego, La Jolla, CA 92037, USA cDepartment of Ophthalmology, Duke University School of Medicine, Albert Eye Research Institute, Durham, NC 27710, USA dThe University of New South Wales, Biotechnology and Biomedical Sciences, Sydney, NSW 2052, Australia NIH-PA Author Manuscript eDepartment of Immunology and Microbial Science, The Scripps Research Institute, La Jolla, CA 92037, USA Abstract NIH-PA Author Manuscript The term interferon describes a family of proteins consisting of three major types (I, II, III) which differ in their primary protein sequences, cognate receptors, genetic loci, and cell types responsible for their production. The interferons, especially types I and II, overlap significantly in the genes they control resulting in a shared spectrum of diverse biological effects which includes regulation of both the innate and adaptive immune responses. As such, the interferons are major effectors in the pathogenesis of autoimmunity, especially systemic autoimmunity. The type I IFNs, because they are produced during the early stages of the innate immune response, are thought to play the foremost role in autoimmune responses. However, numerous studies have found that the single type II IFN, IFN-γ, plays an essential role in the development and severity of systemic autoimmunity, particularly systemic lupus erythematosus. This is supported by animal studies where IFN-γ is uniformly required in both spontaneous and induced models of lupus. Although expression of IFN-γ in cells of the innate immune system is almost immediate after activation, expression in adaptive immunity requires a complex orchestration of cellular interactions, signaling events and epigenetic modifications. The multifaceted nature of IFN-γ in adaptive immunity identifies numerous possible therapeutic targets that, because of the essential contribution of IFN-γ to systemic autoimmunity, have the potential for producing significant benefits. Introduction The term interferon (IFN) was first coined in 1957 to describe a factor with the ability to interfere with the growth of live influenza virus (Isaacs & Lindenmann, 1957). Since then, it was found that the IFNs are a family of proteins consisting of three major types; Type I (IFN-α, -β, -ε, -ω), Type II (IFN-γ), and Type III (IFN-λ1, IFN-λ2 and IFN-λ3, also called IL-29, IL-28A and IL-28B respectively) (Meyer, 2009). All three major types differ in their Corresponding Author: K. Michael Pollard, PhD. Department of Molecular and Experimental Medicine MEM125, The Scripps Research Institute, 10550 North Torrey Pines Road, La Jolla, CA 92037. Tel: 858 784 9124, Fax: 858 784 8836, [email protected]. Disclosure The authors report no conflict of interest. Pollard et al. Page 2 primary protein sequences, cognate receptors, genetic loci, and cell types responsible for their production (Table 1). NIH-PA Author Manuscript Together the interferons influence a wide variety of biological responses including providing protection from viral and bacterial infections, anti-tumor effects, and regulation of effector cells in both innate and adaptive immune responses (Baccala et al., 2005; Hertzog et al., 2011). Included among this diverse spectrum, are a significant amount of shared biological effects due to a remarkable overlap in the many hundreds of genes regulated by the different types of interferon, especially types I and II (Hertzog et al., 2011). Indeed, almost 70% of genes regulated by IFN-γ are also regulated by type I IFN (Hertzog et al., 2011). Such redundancy may be explained by the use of some of the same components of the JAK (Janus kinase)-STAT (signal transducer and activator of transcripton) signaling pathways (Hu & Ivashkiv, 2009; O’Shea & Plenge, 2012). Of the remaining non redundant genes affected by IFN-γ, over 2/3 are inducible and the remainder are repressed. Thus, although overlapping considerably with the type I IFN response, IFN-γ uniquely regulates a significant number of genes, many of which contribute to the particular actions of IFN-γ in host defense, inflammation and autoimmune disease (Billiau & Matthys, 2009). In this review we will address the biology of IFN-γ and the contribution of IFN-γ to the development and pathogenesis of systemic autoimmunity in both humans and animal models. NIH-PA Author Manuscript IFN-γ biology IFN-γ, is secreted predominantly by T cells and natural killer (NK) cells (Billiau & Matthys, 2009) and, to a lesser extent, by other cell types such as macrophages, dendritic cells (DC) and B cells (Meyer, 2009) (Table 1). The broad array of IFN-γ responses are mediated by the cell-specific expression of many hundreds of IFN-γ-regulated genes (Hertzog et al., 2011), for which functional classification encompasses inflammatory mediators, signaling molecules, transcriptional activators, mediators of apoptosis and immune modulators (de Veer et al., 2001). Further adding to the pleiotropic nature of the IFN-γ response are the variety of cell types that possess the IFN-γ receptor (IFN-γR) and the molecular events that constitute IFN-γ-dependent signaling pathways (Hu & Ivashkiv, 2009; Stark et al., 1998). NIH-PA Author Manuscript During innate immune responses IFN-γ is produced by NK and natural killer T (NKT) cells (Schoenborn & Wilson, 2007) as well as macrophages and DCs (Meyer, 2009). In adaptive immunity it is produced by CD8+ T cells in the control of infection, and by the CD4+ T helper 1 (Th1) subset, which promotes inflammatory responses, clearance of intracellular pathogens and class-switching to IgG2a, IgG2b and IgG3 (Baudino et al., 2006; Szabo et al., 2003). IFN-γ is one of the main cytokines that distinguishes Th1 from other CD4+ subsets, including Th2, Th17, follicular T helper (Tfh) and T regulatory (Treg) cells (Zhu et al., 2010). Differentiation of CD4+ T cells to the Th1 subset is driven primarily by IL-12 in the absence of IL-4 and TGF-β (Zhu et al., 2010). Subsequently, IFN-γ production is sustained in this subset by many factors, including IL-12, IL-18, IL-27, and Stat4 (Murphy & Stockinger, 2010; Paunovic et al., 2008; Szabo et al., 2003). Regulation of IFN-γ expression Regulation of IFN-γ expression in innate and adaptive immune responses has been extensively reviewed elsewhere (Aune et al., 2013; Schoenborn & Wilson, 2007) and only a basic outline will be presented here. We will discuss in greater detail more recent information suggesting that long non-coding RNAs (lncRNAs) play a significant role in IFN-γ transcription. Discov Med. Author manuscript; available in PMC 2014 September 01. Pollard et al. Page 3 Transcription and epigenetics NIH-PA Author Manuscript Epigenetic regulation is an important mechanism of transcriptional activation or repression of the Ifng locus (encoding IFN-γ) in innate and adaptive immune responses (Aune et al., 2013; Schoenborn & Wilson, 2007). Regulation of IFN-γ involves epigenetic modifications in the promoter region, conserved non-coding sequences such as CNS-6 and CNS-22 that help regulate IFN-γ expression in Th1 CD4+ T cells (Schoenborn & Wilson, 2007), and binding of T-box transcription factor TBX21 (T-bet) which directs Th1 lineage commitment (Beima et al., 2006; Schoenborn & Wilson, 2007). IFN-γ expressing cells involved in the innate immune response such as NK and NKT cells rapidly produce the cytokine due to constitutive expression of transcription factors Eomes and T-bet (NK cells) or T-bet alone (NKT) which are able to bind to regulatory elements that are already accessible within the Ifng locus, leading to activation of Ifng transcription. In contrast, IFN-γ expression by CD4+ and CD8+ T cells in adaptive immune responses requires induction of T-bet as well as epigenetic modifications within the Ifng gene that make regulatory elements accessible to T-bet and other transcription factors. This differentiation process of naïve CD4+ or CD8+ T cells to Th1 or cytotoxic T effector cells requires T cell receptor (TCR) stimulation and multiple rounds of cell division (Aune et al., 2013; Schoenborn & Wilson, 2007). NIH-PA Author Manuscript lncRNA Within the last eight years, it has become apparent that anti-sense non-coding RNAs (ncRNAs) operate as an endogenous cellular mechanism to selectively regulate gene transcription (Hawkins & Morris, 2008). While there are several distinct mechanisms by which ncRNAs affect gene expression, one mechanism in particular involves anti-sense long non-coding RNAs (lncRNAs) that function to specifically recruit epigenetic silencing complexes to homology containing loci (Hawkins & Morris, 2010; Johnsson et al., 2013; Morris et al., 2008; Yu et al., 2008). These antisense lncRNAs are distinct from small noncoding RNA effector molecules such as microRNAs (miRNAs) and piwi associated RNAs (piRNAs) (Hartig et al., 2007), which function predominantly through the RNAi posttranscriptional silencing pathway. Although significant advances have been made in defining the role of miRNAs and piRNAs in gene regulation, far less is known about the extent of lncRNAs in regulating gene transcription. NIH-PA Author Manuscript Recently, the lncRNA Tmevpg1 (also known as NeST) was shown to positively contribute to IFN-γ production by CD4+ and CD8+ T cells (Collier et al., 2012; Gomez et al., 2013). Tmevpg1 is adjacent to the Ifng gene in both mice and humans and is encoded on the DNA strand opposite to that coding IFN-γ. Tmevpg1 transcription is dependent upon transcription factors Stat4 and T-bet, which also influence Ifng transcription in CD4+ Th1 T cells. Significantly, transfection of Tmevpg1 alone cannot increase IFN-γ protein in Th0, Th1 or Th2 cells (Collier et al., 2012). However, mice transgenic for Tmevpg1 have increased IFNγ and are protected from Salmonella infection arguing, that in vivo, Tmevpg1 can act in trans to regulate target gene expression (Gomez et al., 2013) similar to other observations of antisense lncRNA trans directed epigenetic regulation of gene expression (Hawkins & Morris, 2010; Johnsson et al., 2013; Morris et al., 2008; Yu et al., 2008). These studies show that IFN-γ expression is essentially unregulated in innate immune responses resulting in almost immediate production of the cytokine. However, any ensuing IFN-γ driven adaptive immune response requires a much more complex orchestration of cellular interactions and signaling events. The recent discovery that the lncRNA Tmevpg1 regulates IFN-γ expression in T cells suggests it could be used as a target to deduce the Discov Med. Author manuscript; available in PMC 2014 September 01. Pollard et al. Page 4 relative importance of innate or adaptive immune system production of IFN--γ in disease processes including autoimmunity. NIH-PA Author Manuscript IFN-γ in autoimmunity NIH-PA Author Manuscript IFNs are major effectors in the pathogenesis of autoimmunity (Baccala et al., 2005). In recent years type I IFN production has been argued to be central to the pathogenesis of systemic autoimmunity (Baccala et al., 2007; Ronnblom & Eloranta, 2013). This is based on the observation of increased expression of type I IFN inducible genes in peripheral blood cells, and is commonly called the type I IFN gene signature (Obermoser & Pascual, 2010; Ronnblom & Eloranta, 2013). The type I IFN signature is found in patients with systemic lupus erythematosus (SLE), Sjögren’s syndrome (SS), polymyositis (PM), dermatomyositis (DM) and systemic sclerosis (SSc), but less frequently in patients with rheumatoid arthritis (RA) and multiple sclerosis (Ronnblom & Eloranta, 2013). A type I IFN signature, defined by five genes (IFI44, IFI44L, IFI27, RSAD2 and IFI6) has been shown to correlate with disease activity and disease-affected tissue in SLE, DM, PM, and SSc (Higgs et al., 2011). However, due to the significant overlap between the genes induced by IFN types I and II it has proven difficult to differentiate which IFNs are the major contributors to systemic autoimmune pathogenesis (Gottenberg et al., 2006; Hall et al., 2012; Nguyen & Peck, 2013; Wong et al., 2012). For example most members of the type I IFN signature described above are also induced by IFN-γ (Hall et al., 2012). Moreover it must be appreciated that even genes preferentially induced by IFN-γ (Hall et al., 2012) can also be induced by other proinflammatory cytokines (Lubeseder-Martellato et al., 2002). However, as type I IFN is initiated in the early stages of the innate immune response, and is argued to amplify the adaptive (auto)immune response, it has been suggested that it plays the dominant role (Baccala et al., 2007). Nonetheless, given the significant overlap in gene expression driven by IFN types I and II (de Veer et al., 2001; Hall et al., 2012; Hertzog et al., 2011) it is not surprising that numerous studies have established that type II IFN (IFN-γ) also plays a pivotal role in the development and severity of autoimmune diseases (Baccala et al., 2005; Hu & Ivashkiv, 2009; Meyer, 2009). NIH-PA Author Manuscript The mechanism whereby IFN-γ leads to systemic autoimmunity remains unclear, however, the importance of IFN-γ to T cell differentiation and immunoglobulin class switching in B cells underlines a substantial contribution to adaptive immune responses in autoimmunity. Increased IFN-γ expression alone can result in the development of systemic autoimmunity as documented by the finding that epidermal transgenic expression of IFN-γ leads to antidsDNA and anti-histone autoantibodies and glomerulonephritis (Seery, 2000). However, location of transgenic IFN-γ expression is important as expression in other sites, such as pancreatic islets and neuromuscular junction, does not lead to systemic autoimmunity (Seery, 2000). The ability of IFN-γ to promote B cell IgG class switching to more pathogenic (IgG2a and IgG3 in mice) autoantibodies and activation of IgG Fc receptors and complement (Baudino et al., 2006) likely also contributes to disease severity. IFN-γ also plays a significant role in end organ damage due to infiltration of IFN-γ secreting T cells resulting in macrophage activation, inflammation and tissue damage (Hu & Ivashkiv, 2009; Schwarting et al., 1998). The Th1 associated chemokine receptor CXCR3 is increased in lupus nephritis and may contribute to tissue inflammation and autoantibody production (Lacotte et al., 2013). Mutation of ROQUIN (Rc3h1) in Roquinsan/san mice, another model of lupus, leads to reduced decay of IFN-γ mRNA resulting in increased IFN-γ signaling and accumulation of follicular helper T (Tfh) cells, culminating in increased germinal center B cells and autoantibodies (Lee et al., 2012). Notably in these mutant mice, IFN-γR-deficiency prevented the development of lupus, whereas deficiency of ICOS, previously thought to be the cause autoimmunity in this model because of high levels of expression in Tfh cells, did not. The above findings provide an attractive mechanism to explain the role of IFN-γ in Discov Med. Author manuscript; available in PMC 2014 September 01. Pollard et al. Page 5 NIH-PA Author Manuscript adaptive (auto)immunity as it directly links expansion of IFN-γ producing CD4+ T cells with autoantibody production. However, the relevance of this pathway to human SLE or other murine lupus models will need to investigated. Human idiopathic systemic autoimmunity IFN-γ has been shown to be a prominent participant in human systemic autoimmune responses (Theofilopoulos et al., 2001) (Table 2).This is most convincingly seen in patients with SLE. IFN-γ mRNA is increased in peripheral blood mononuclear cells (PBMC) (Csiszar et al., 2000; Harigai et al., 2008) and correlates with PBMC mRNA expression of its transcription factor T-bet (Lit et al., 2007). Elevated protein levels of IFN-γ have been found in serum (Funauchi et al., 1991) and following in vitro stimulation of PBMC (Harigai et al., 2008). Serum IFN-γ correlates with disease activity (Funauchi et al., 1991) and increased IFN-γ/IL-4 ratio is found in patients with nephritis (Akahoshi et al., 1999; Masutani et al., 2001). NIH-PA Author Manuscript An established role for IFN-γ in other systemic autoimmune diseases is less convincing. Increased IFN-γ has been found in the PBMC of primary SS patients with Raynaud’s phenomenon (Willeke et al., 2009) but not those with SS alone (Funauchi et al., 1991; Willeke et al., 2009). Indeed, although the IFN signature has been found in SS (Ronnblom & Eloranta, 2013), demonstration of increased IFN-α/β or IFN-γ in primary SS has proven difficult (Hjelmervik et al., 2005). However, a more recent study has suggested that the IFN signature in salivary glands of SS shows a predominant IFN-γ response (Hall et al., 2012). In the idiopathic inflammatory myopathies the IFN-γ/IL-4 ratio is lower in peripheral blood CD4+ T cells in DM than PM (Ishii et al., 2008) even though IFN-γ levels correlate with activation of IFN-induced genes in the skin of DM patients (Wong et al., 2012). This dichotomy may reflect the pronounced infiltration of activated CD4+ T cells in DM skin (Caproni et al., 2004). A recent study of cytokine expression in systemic sclerosis found increased IFN-γ positive CD4+ T cells and increased T cell secretion of IFN-γ in a subgroup of patients with limited cutaneous SSc (Radstake et al., 2009). Animal models of idiopathic systemic autoimmunity NIH-PA Author Manuscript Studies of murine models of spontaneous SLE strongly support the importance of IFN-γ in systemic autoimmune disease particularly SLE (Table 3). Increases in IFN-γ are found in lupus-prone mice (Prud’homme et al., 1995) and correlate with disease progression (Enghard et al., 2006). NZB/W F1 mice treated with IFN-γ have accelerated disease while treatment with anti-IFN-γ mAb results in disease remission (Jacob et al., 1987). Injection of cDNA encoding the receptor of IFN-γ (IFN-γR) (Lawson et al., 2000) or treatment with soluble IFN-γR (Ozmen et al., 1995) reduces serum levels of IFN-γ and manifestations of disease in MRL-Faslpr and NZB/W F1 mice respectively. Genetic deficiency of IFN-γR in NZB/W F1 mice reduces production of auto-antibodies and glomerulonephritis (Haas et al., 1998) and protects MRL-Faslpr mice from lymphadenopathy, autoantibodies and renal disease (Hron & Peng, 2004). Absence of IFN-γ also dramatically reduces lymphadenopathy, anti-dsDNA autoantibodies and glomerulonephritis in MRL-Faslpr mice (Balomenos et al., 1998). In contrast, type I IFN in MRL-Faslpr mice is not required for development of autoimmune disease. In the absence of type I IFN signaling lymphoproliferation, autoantibodies and end organ disease were more severe (Hron & Peng, 2004), antagonistic anti-IFNαR antibodies had minimal effect (Baccala et al., 2012), and in another study, type I IFN was required for sex (female) dependent proteinuria although not for renal infiltrates or glomerular score (Nickerson et al., 2013). Notably serum IgG and anti-nucleosome autoantibodies were not Discov Med. Author manuscript; available in PMC 2014 September 01. Pollard et al. Page 6 NIH-PA Author Manuscript dependent upon type I IFN in the latter study. Although these findings may reflect use of different substrains of MRL-Faslpr mice (Nickerson et al., 2013) they are clearly different from the profound reduction in disease in the absence of IFN-γ (Balomenos et al., 1998). In support of the prominence of IFN-γ in pathogenesis of SS (Hall et al., 2012), NOD/ShiLtJ mice, a model of Sjögren’s syndrome, have increased levels of IFN-γ and lack of IFN-γ or IFN-γR inhibits disease including reduction of glandular infiltrates, and autoantibodies including anti-nuclear autoantibodies (ANA) (Cha et al., 2004; Nguyen & Peck, 2013). IFN-γ in induced systemic autoimmunity NIH-PA Author Manuscript IFN-γ has also been found to be required for animal models of induced systemic autoimmunity (Table 3). Mercury exposure in mice elicits systemic autoimmunity characterized by T and B cell activation, hypergammaglobulinemia, ANA, and immune complex deposits, all of which are abrogated by the absence of IFN-γ (Pollard et al., 2010). The importance of IFN-γ to murine mercury-induced autoimmunity (mHgIA) is supported by a study of mice deficient in genes regulating IFN-γ expression (Casp1, Nlrp3, Il12a, Il12b, Stat4) or function (Ifngr1, Irf1), which revealed that absence of either Ifngr1 or Irf1 resulted in a striking reduction of disease, while deficiency of genes promoting IFN-γ expression had modest to no effect (Pollard et al., 2012). Our preliminary studies (Pollard & Kono, 2013) suggest that type I IFN is not required for mHgIA. These findings argue that IFN-γ signaling pathways predominate in mHgIA. The naturally occurring hydrocarbon oil TMPD (2,6,10,14-tetramethylpentadecane), more commonly known as pristane, induces a severe form of SLE in mice which includes female predominance, ANA, nephritis, arthritis and pulmonary vasculitis (Pollard et al., 2010). In the absence of IFN-γ, pristane treated mice have significant reduction in serum immunoglobulin, ANA, kidney immune deposits and proteinuria compared to wild type mice (Richards et al., 2001). Type I IFN was also required for pristane-induced autoimmunity, however, in type I IFN receptor (Ifnar) deficient mice renal deposits were not affected and although levels of ANA were less than wild type mice, all were ANA positive. (Nacionales et al., 2007). Thus, as for lupus-prone MRL-Faslpr mice and mHgIA, deficiency of IFN-γ appears to have more profound effects on the spectrum of disease expression than absence of type I IFN signaling. Attempts to induce/exacerbate disease in lupus mice deficient in type I IFN with IFN-γ and vice versa would help resolve which IFN type is of greater importance to disease severity. We are unaware of any studies that address this issue. NIH-PA Author Manuscript The role of IFN-γ in animal models of induced RA is controversial. IFN-γ is protective in collagen-induced arthritis in the presence of CFA but not in its absence (Schurgers et al., 2011). This protective effect of IFN-γ is most often seen in experimental models which use complete Freund’s adjuvant such as collage-induced arthritis, experimental autoimmune encephalomyelitis and experimental autoimmune uveitis. It has been proposed that the inhibition of development of Th17 cells by IFN-γ contributes to this protective effect (Kelchtermans et al., 2008). In contrast the earlier onset and more severe arthritis produced following immunization with glucose-6-phosphate isomerase (G6PI) does require IFN-γ even in the presence of CFA (Schurgers et al., 2011). Thus the multiple pathways that lead to experimental arthritis can have different requirements for IFN-γ. Therapeutic targets Even though a number of therapeutic approaches have been identified to control IFN-γ and related cytokines (Chugh, 2012; Hayashi, 2010) little has been done to develop therapies targeting IFN-γ in systemic autoimmune diseases. This may stem from the fact that human deficiency of IFN-γ is associated with severe infection (Meyer, 2009). Even so several Discov Med. Author manuscript; available in PMC 2014 September 01. Pollard et al. Page 7 NIH-PA Author Manuscript efforts have and are being made to determine the effectiveness of anti-IFN-γ therapy. Fontolizumab, a humanized monoclonal antibody against IFN-γ, was well tolerated and showed some efficacy in patients with Crohn’s Disease (Reinisch et al., 2010) however a phase II clinical trial investigating its use in rheumatoid arthritis was terminated because the first phase did not meet the endpoint (ClinicalTrials.gov). Amgen’s product pipeline includes AMG 811, a human monoclonal antibody that inhibits IFN-γ. It is being evaluated in safety trials with subjects with discoid lupus and subjects with systemic lupus erythematosus with and without glomerulonephritis (ClinicalTrials.gov). Such non-specific targeting of IFN-γ is likely to impact both innate and adaptive immunity. Given the important role that IFN-γ plays in adaptive autoimmune responses therapy targeted to cellular components regulating IFN-γ expression in T cells, such as the lncRNA Tmevpg1, may provide greater therapeutic benefit without adverse effect on innate responses to infection. Conclusion NIH-PA Author Manuscript Numerous studies highlight the pivotal role that both type I and II IFN play in systemic autoimmunity in humans and spontaneous and induced animal models. While considerable focus has been placed on the type I IFN signature it is clear that the extensive overlap among genes induced by IFNs highlights the difficulty in identifying which IFN type has the predominant activity in inducing disease. Studies of IFN-γ in SLE provide strong evidence for its role in disease including the adaptive immune response, inflammation, and end organ damage mediated by infiltrating IFN-γ+ T cells. This is supported by studies in animal models of SLE which demonstrate the essential role of IFN-γ in both spontaneous and induced lupus-like disease. These studies suggest that greater thought needs to be given to therapeutic regulation of IFN-γ in SLE. Acknowledgments This work was supported in part by NIH grants ES014847, ES007511, ES020388 (KMP), AI099783 (KVM). References NIH-PA Author Manuscript Akahoshi M, Nakashima H, Tanaka Y, Kohsaka T, Nagano S, Ohgami E, Arinobu Y, Yamaoka K, Niiro H, Shinozaki M, Hirakata H, Horiuchi T, Otsuka T, Niho Y. Th1/Th2 balance of peripheral T helper cells in systemic lupus erythematosus. Arthritis Rheum. 1999; 42(8):1644–1648. [PubMed: 10446863] Aune TM, Collins PL, Collier SP, Henderson MA, Chang S. Epigenetic Activation and Silencing of the Gene that Encodes IFN-gamma. Frontiers in immunology. 2013; 4:112. [PubMed: 23720660] Baccala R, Gonzalez-Quintial R, Schreiber RD, Lawson BR, Kono DH, Theofilopoulos AN. AntiIFN-alpha/beta Receptor Antibody Treatment Ameliorates Disease in Lupus-Predisposed Mice. J Immunol. 2012; 189(12):5976–5984. [PubMed: 23175700] Baccala R, Hoebe K, Kono DH, Beutler B, Theofilopoulos AN. TLR-dependent and TLR-independent pathways of type I interferon induction in systemic autoimmunity. Nat Med. 2007; 13(5):543–551. [PubMed: 17479100] Baccala R, Kono DH, Theofilopoulos AN. Interferons as pathogenic effectors in autoimmunity. Immunol Rev. 2005; 204:9–26. [PubMed: 15790347] Balomenos D, Rumold R, Theofilopoulos AN. Interferon-gamma is required for lupus-like disease and lymphoaccumulation in MRL-lpr mice. J Clin Invest. 1998; 101(2):364–371. [PubMed: 9435308] Baudino L, Azeredo Da Silveira S, Nakata M, Izui S. Molecular and cellular basis for pathogenicity of autoantibodies: lessons from murine monoclonal autoantibodies. Springer Semin Immunopathol. 2006; 28(2):175–184. Discov Med. Author manuscript; available in PMC 2014 September 01. Pollard et al. Page 8 NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript Beima KM, Miazgowicz MM, Lewis MD, Yan PS, Huang TH, Weinmann AS. T-bet binding to newly identified target gene promoters is cell type-independent but results in variable context-dependent functional effects. J Biol Chem. 2006; 281(17):11992–12000. [PubMed: 16473879] Billiau A, Matthys P. Interferon-gamma: a historical perspective. Cytokine Growth Factor Rev. 2009; 20(2):97–113. Caproni M, Torchia D, Cardinali C, Volpi W, Del Bianco E, D’agata A, Fabbri P. Infiltrating cells, related cytokines and chemokine receptors in lesional skin of patients with dermatomyositis. Br J Dermatol. 2004; 151(4):784–791. Cha S, Brayer J, Gao J, Brown V, Killedar S, Yasunari U, Peck AB. A dual role for interferon-gamma in the pathogenesis of Sjogren’s syndrome-like autoimmune exocrinopathy in the nonobese diabetic mouse. Scand J Immunol. 2004; 60(6):552–565. Chugh PK. Lupus: novel therapies in clinical development. Eur J Intern Med. 2012; 23(3):212–218. [PubMed: 22385876] Collier SP, Collins PL, Williams CL, Boothby MR, Aune TM. Cutting edge: influence of Tmevpg1, a long intergenic noncoding RNA, on the expression of Ifng by Th1 cells. J Immunol. 2012; 189(5): 2084–2088. Csiszar A, Nagy G, Gergely P, Pozsonyi T, Pocsik E. Increased interferon-gamma (IFN-gamma), IL-10 and decreased IL-4 mRNA expression in peripheral blood mononuclear cells (PBMC) from patients with systemic lupus erythematosus (SLE). Clin Exp Immunol. 2000; 122(3):464–470. De Veer MJ, Holko M, Frevel M, Walker E, Der S, Paranjape JM, Silverman RH, Williams BR. Functional classification of interferon-stimulated genes identified using microarrays. J Leukoc Biol. 2001; 69(6):912–920. Enghard P, Langnickel D, Riemekasten G. T cell cytokine imbalance towards production of IFNgamma and IL-10 in NZB/W F1 lupus-prone mice is associated with autoantibody levels and nephritis. Scand J Rheumatol. 2006; 35(3):209–216. [PubMed: 16766368] Funauchi M, Sugishima H, Minoda M, Horiuchi A. Serum level of interferon-gamma in autoimmune diseases. Tohoku J Exp Med. 1991; 164(4):259–267. Gomez JA, Wapinski OL, Yang YW, Bureau JF, Gopinath S, Monack DM, Chang HY, Brahic M, Kirkegaard K. The NeST long ncRNA controls microbial susceptibility and epigenetic activation of the interferon-gamma locus. Cell. 2013; 152(4):743–754. [PubMed: 23415224] Gottenberg JE, Cagnard N, Lucchesi C, Letourneur F, Mistou S, Lazure T, Jacques S, Ba N, Ittah M, Lepajolec C, Labetoulle M, Ardizzone M, Sibilia J, Fournier C, Chiocchia G, Mariette X. Activation of IFN pathways and plasmacytoid dendritic cell recruitment in target organs of primary Sjogren’s syndrome. Proc Natl Acad Sci U S A. 2006; 103(8):2770–2775. [PubMed: 16477017] Haas C, Ryffel B, Le Hir M. IFN-gamma receptor deletion prevents autoantibody production and glomerulonephritis in lupus-prone (NZB x NZW)F1 mice. J Immunol. 1998; 160(8):3713–3718. Hall JC, Casciola-Rosen L, Berger AE, Kapsogeorgou EK, Cheadle C, Tzioufas AG, Baer AN, Rosen A. Precise probes of type II interferon activity define the origin of interferon signatures in target tissues in rheumatic diseases. Proc Natl Acad Sci U S A. 2012; 109(43):17609–17614. [PubMed: 23045702] Harigai M, Kawamoto M, Hara M, Kubota T, Kamatani N, Miyasaka N. Excessive production of IFNgamma in patients with systemic lupus erythematosus and its contribution to induction of B lymphocyte stimulator/B cell-activating factor/TNF ligand superfamily-13B. J Immunol. 2008; 181(3):2211–2219. [PubMed: 18641361] Hartig JV, Tomari Y, Forstemann K. piRNAs--the ancient hunters of genome invaders. Genes Dev. 2007; 21(14):1707–1713. [PubMed: 17639076] Hawkins PG, Morris KV. RNA and transcriptional modulation of gene expression. Cell Cycle. 2008; 7(5):602–607. [PubMed: 18256543] Hawkins PG, Morris KV. Transcriptional regulation of Oct4 by a long non-coding RNA antisense to Oct4-pseudogene 5. Transcription. 2010; 1(3):165–175. Hayashi T. Therapeutic strategies for SLE involving cytokines: mechanism-oriented therapies especially IFN-gamma targeting gene therapy. J Biomed Biotechnol. 2010; 2010 Discov Med. Author manuscript; available in PMC 2014 September 01. Pollard et al. Page 9 NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript Hertzog P, Forster S, Samarajiwa S. Systems biology of interferon responses. J Interferon Cytokine Res. 2011; 31(1):5–11. [PubMed: 21226606] Higgs BW, Liu Z, White B, Zhu W, White WI, Morehouse C, Brohawn P, Kiener PA, Richman L, Fiorentino D, Greenberg SA, Jallal B, Yao Y. Patients with systemic lupus erythematosus, myositis, rheumatoid arthritis and scleroderma share activation of a common type I interferon pathway. Ann Rheum Dis. 2011; 70(11):2029–2036. Hjelmervik TO, Petersen K, Jonassen I, Jonsson R, Bolstad AI. Gene expression profiling of minor salivary glands clearly distinguishes primary Sjogren’s syndrome patients from healthy control subjects. Arthritis Rheum. 2005; 52(5):1534–1544. [PubMed: 15880807] Hron JD, Peng SL. Type I IFN protects against murine lupus. J Immunol. 2004; 173(3):2134–2142. [PubMed: 15265950] Hu X, Ivashkiv LB. Cross-regulation of signaling pathways by interferon-gamma: implications for immune responses and autoimmune diseases. Immunity. 2009; 31(4):539–550. [PubMed: 19833085] Isaacs A, Lindenmann J. Virus interference. I. The interferon. Proceedings of the Royal Society of London. Series B, Containing papers of a Biological character. Royal Society. 1957; 147(927): 258–267. Ishii W, Matsuda M, Shimojima Y, Itoh S, Sumida T, Ikeda S. Flow cytometric analysis of lymphocyte subpopulations and TH1/TH2 balance in patients with polymyositis and dermatomyositis. Intern Med. 2008; 47(18):1593–1599. [PubMed: 18797118] Jacob CO, Van Der Meide PH, Mcdevitt HO. In vivo treatment of (NZB X NZW)F1 lupus-like nephritis with monoclonal antibody to gamma interferon. J Exp Med. 1987; 166(3):798–803. Johnsson P, Ackley A, Corcoran M, Vidarsdottir L, Grander D, Morris KV. A novel pseudogene noncoding RNA network regulates PTEN transcription and translation in human cells. Nature Structural & Molecular Biology. 2013 In Press. Kelchtermans H, Billiau A, Matthys P. How interferon-gamma keeps autoimmune diseases in check. Trends Immunol. 2008; 29(10):479–486. [PubMed: 18775671] Lacotte S, Decossas M, Le Coz C, Brun S, Muller S, Dumortier H. Early differentiated CD138(high) MHCII+ IgG+ plasma cells express CXCR3 and localize into inflamed kidneys of lupus mice. PLoS One. 2013; 8(3):e58140. [PubMed: 23520491] Lawson BR, Prud’homme GJ, Chang Y, Gardner HA, Kuan J, Kono DH, Theofilopoulos AN. Treatment of murine lupus with cDNA encoding IFN-gammaR/Fc. J Clin Invest. 2000; 106(2): 207–215. Lee SK, Silva DG, Martin JL, Pratama A, Hu X, Chang PP, Walters G, Vinuesa CG. Interferongamma excess leads to pathogenic accumulation of follicular helper T cells and germinal centers. Immunity. 2012; 37(5):880–892. [PubMed: 23159227] Lit LC, Wong CK, Li EK, Tam LS, Lam CW, Lo YM. Elevated gene expression of Th1/Th2 associated transcription factors is correlated with disease activity in patients with systemic lupus erythematosus. J Rheumatol. 2007; 34(1):89–96. [PubMed: 17117487] Lubeseder-Martellato C, Guenzi E, Jorg A, Topolt K, Naschberger E, Kremmer E, Zietz C, Tschachler E, Hutzler P, Schwemmle M, Matzen K, Grimm T, Ensoli B, Sturzl M. Guanylate-binding protein-1 expression is selectively induced by inflammatory cytokines and is an activation marker of endothelial cells during inflammatory diseases. Am J Pathol. 2002; 161(5):1749–1759. [PubMed: 12414522] Masutani K, Akahoshi M, Tsuruya K, Tokumoto M, Ninomiya T, Kohsaka T, Fukuda K, Kanai H, Nakashima H, Otsuka T, Hirakata H. Predominance of Th1 immune response in diffuse proliferative lupus nephritis. Arthritis Rheum. 2001; 44(9):2097–2106. [PubMed: 11592372] Meyer O. Interferons and autoimmune disorders. Joint Bone Spine. 2009; 76(5):464–473. [PubMed: 19773191] Morris KV, Santoso S, Turner AM, Pastori C, Hawkins PG. Bidirectional transcription directs both transcriptional gene activation and suppression in human cells. PLoS Genet. 2008; 4(11):e1000258. [PubMed: 19008947] Murphy KM, Stockinger B. Effector T cell plasticity: flexibility in the face of changing circumstances. Nat Immunol. 2010; 11(8):674–680. [PubMed: 20644573] Discov Med. Author manuscript; available in PMC 2014 September 01. Pollard et al. Page 10 NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript Nacionales DC, Kelly-Scumpia KM, Lee PY, Weinstein JS, Lyons R, Sobel E, Satoh M, Reeves WH. Deficiency of the type I interferon receptor protects mice from experimental lupus. Arthritis Rheum. 2007; 56(11):3770–3783. [PubMed: 17968932] Nguyen CQ, Peck AB. The Interferon-Signature of Sjogren’s Syndrome: How Unique Biomarkers Can Identify Underlying Inflammatory and Immunopathological Mechanisms of Specific Diseases. Frontiers in immunology. 2013; 4:142. Nickerson KM, Cullen JL, Kashgarian M, Shlomchik MJ. Exacerbated autoimmunity in the absence of TLR9 in MRL.Fas(lpr) mice depends on Ifnar1. J Immunol. 2013; 190(8):3889–3894. O’shea JJ, Plenge R. JAK and STAT signaling molecules in immunoregulation and immune-mediated disease. Immunity. 2012; 36(4):542–550. Obermoser G, Pascual V. The interferon-alpha signature of systemic lupus erythematosus. Lupus. 2010; 19(9):1012–1019. [PubMed: 20693194] Ozmen L, Roman D, Fountoulakis M, Schmid G, Ryffel B, Garotta G. Experimental therapy of systemic lupus erythematosus: the treatment of NZB/W mice with mouse soluble interferongamma receptor inhibits the onset of glomerulonephritis. Eur J Immunol. 1995; 25(1):6–12. Paunovic V, Carroll HP, Vandenbroeck K, Gadina M. Signalling, inflammation and arthritis: crossed signals: the role of interleukin (IL)-12, -17, -23 and -27 in autoimmunity. Rheumatology (Oxford). 2008; 47(6):771–776. [PubMed: 18238793] Pollard KM, Hultman P, Kono DH. Toxicology of autoimmune diseases. Chem Res Toxicol. 2010; 23(3):455–466. Pollard KM, Hultman P, Toomey CB, Cauvi DM, Hoffman HM, Hamel JC, Kono DH. Definition of IFN-gamma-related pathways critical for chemically-induced systemic autoimmunity. J Autoimmun. 2012; 39(4):323–331. [PubMed: 22578563] Pollard KM, Kono DH. Requirements for innate immune pathways in environmentally induced autoimmunity. BMC medicine. 2013; 11:100. [PubMed: 23557436] Prud’homme GJ, Kono DH, Theofilopoulos AN. Quantitative polymerase chain reaction analysis reveals marked overexpression of interleukin-1 beta, interleukin-1 and interferon-gamma mRNA in the lymph nodes of lupus-prone mice. Mol Immunol. 1995; 32(7):495–503. [PubMed: 7783752] Radstake TR, Van Bon L, Broen J, Hussiani A, Hesselstrand R, Wuttge DM, Deng Y, Simms R, Lubberts E, Lafyatis R. The pronounced Th17 profile in systemic sclerosis (SSc) together with intracellular expression of TGFbeta and IFNgamma distinguishes SSc phenotypes. PLoS One. 2009; 4(6):e5903. Reinisch W, De Villiers W, Bene L, Simon L, Racz I, Katz S, Altorjay I, Feagan B, Riff D, Bernstein CN, Hommes D, Rutgeerts P, Cortot A, Gaspari M, Cheng M, Pearce T, Sands BE. Fontolizumab in moderate to severe Crohn’s disease: a phase 2, randomized, double-blind, placebo-controlled, multiple-dose study. Inflamm Bowel Dis. 2010; 16(2):233–242. [PubMed: 19637334] Richards HB, Satoh M, Jennette JC, Croker BP, Yoshida H, Reeves WH. Interferon-gamma is required for lupus nephritis in mice treated with the hydrocarbon oil pristane. Kidney Int. 2001; 60(6): 2173–2180. [PubMed: 11737591] Ronnblom L, Eloranta ML. The interferon signature in autoimmune diseases. Curr Opin Rheumatol. 2013; 25(2):248–253. [PubMed: 23249830] Schoenborn JR, Wilson CB. Regulation of interferon-gamma during innate and adaptive immune responses. Adv Immunol. 2007; 96:41–101. [PubMed: 17981204] Schurgers E, Billiau A, Matthys P. Collagen-induced arthritis as an animal model for rheumatoid arthritis: focus on interferon-gamma. J Interferon Cytokine Res. 2011; 31(12):917–926. [PubMed: 21905879] Schwarting A, Wada T, Kinoshita K, Tesch G, Kelley VR. IFN-gamma receptor signaling is essential for the initiation, acceleration, and destruction of autoimmune kidney disease in MRL-Fas(lpr) mice. J Immunol. 1998; 161(1):494–503. [PubMed: 9647261] Seery JP. IFN-gamma transgenic mice: clues to the pathogenesis of systemic lupus erythematosus? Arthritis Res. 2000; 2(6):437–440. [PubMed: 11094455] Stark GR, Kerr IM, Williams BR, Silverman RH, Schreiber RD. How cells respond to interferons. Annu Rev Biochem. 1998; 67:227–264. Discov Med. Author manuscript; available in PMC 2014 September 01. Pollard et al. Page 11 NIH-PA Author Manuscript Szabo SJ, Sullivan BM, Peng SL, Glimcher LH. Molecular Mechanisms Regulating Th1 Immune Responses. Annu Rev Immunol. 2003; 21:713–758. [PubMed: 12500979] Theofilopoulos AN, Koundouris S, Kono DH, Lawson BR. The role of IFN-gamma in systemic lupus erythematosus: a challenge to the Th1/Th2 paradigm in autoimmunity. Arthritis Res. 2001; 3(3): 136–141. [PubMed: 11299053] Willeke P, Schluter B, Schotte H, Domschke W, Gaubitz M, Becker H. Interferon-gamma is increased in patients with primary Sjogren’s syndrome and Raynaud’s phenomenon. Semin Arthritis Rheum. 2009; 39(3):197–202. Wong D, Kea B, Pesich R, Higgs BW, Zhu W, Brown P, Yao Y, Fiorentino D. Interferon and biologic signatures in dermatomyositis skin: specificity and heterogeneity across diseases. PLoS One. 2012; 7(1):e29161. [PubMed: 22235269] Yu W, Gius D, Onyango P, Muldoon-Jacobs K, Karp J, Feinberg AP, Cui H. Epigenetic silencing of tumour suppressor gene p15 by its antisense RNA. Nature. 2008; 451(7175):202–206. [PubMed: 18185590] Zhu J, Yamane H, Paul WE. Differentiation of effector CD4 T cell populations (*). Annu Rev Immunol. 2010; 28:445–489. [PubMed: 20192806] NIH-PA Author Manuscript NIH-PA Author Manuscript Discov Med. Author manuscript; available in PMC 2014 September 01. NIH-PA Author Manuscript III 1(H), 4(M) 21(H), 16(M) IL10R2 21(H), 16(M) IFNLR1 6(H), 10(M) IFNGR2 21(H), 16(M) 21(H), 16(M) Gene Loci Chr. (Species) IFNGR1 IFNAR2 IFNAR1 Receptor pDCs CD4 and CD8 T cells, NK cells, NKT cells, Macrophages, DCs, B cells Fibroblasts, pDCs pDCs** Cellular Source Abbreviations: DCs dendritic cells, pDCs plasmacytoid dendritic cells, NK natural killer, NKT natural killer T, H human, M mouse Most cells can secrete IFN-α, but pDCs have the greatest capacity ** IFN-ε (1 gene) and IFN-γ (1 gene present in humans, but not mice) are not included. * 12(H), 10(M) γ (1) 19(H), 7(M) 9(H), 4(M) β (1) λ (3) cluster on α (13) I* II Gene Loci Chr.(Species) Class (no. of genes) IFN Type NIH-PA Author Manuscript The three major types of interferon (IFN) NIH-PA Author Manuscript Table 1 Pollard et al. Page 12 Discov Med. Author manuscript; available in PMC 2014 September 01. Pollard et al. Page 13 Table 2 IFN-γ in human systemic autoimmune diseases NIH-PA Author Manuscript Disease IFN-γ Phenotype Reference SLE Increased IFN-γ mRNA in PBMC. Csiszár et al, 2000 Increased IFN-γ in serum of patients with active disease. Funauchi et al, 1991 Increased IFN-γ RNA and protein after anti-CD3/CD28 stimulation of PBMC. Harigai et al, 2008 Increased IFN-γ mRNA in PBMC correlated with T-bet mRNA. IFN-γ/IL-4 ratio correlated with disease activity. Lit et al, 2007 Increased IFN-γ/IL-4 ratio by intracellular flow cytometry in PBMC of patients with diffuse proliferative glomerulonephritis. Akahoshi et al, 1999 Increased IFN-γ/IL-4 ratio in PBMC and increased IFN-γ+ cells in renal biopsy of patients with diffuse proliferative glomerulonephritis . Masutani et al, 2001 Increased IFN-γ secretion of PBMC from SS patients with Raynaud’s phenomenon stimulated with T cell mitogen phytohemagglutinin. Willeke et al, 2009 SS Prominent IFN-γ transcriptional response in SS salivary glands. Hall et al, 2012 DM Increased IFN-γ mRNA in skin of DM patients correlates with IFN transcriptional response in DM skin Wong et al, 2012 SSc Increased IFN-γ by intracellular flow cytometry in T cells of patients with limited SSc. Increased in vitro IFN-γ secretion by T cells of patients with limited SSc. Radstake et al, 2009 NIH-PA Author Manuscript NIH-PA Author Manuscript Discov Med. Author manuscript; available in PMC 2014 September 01. Pollard et al. Page 14 Table 3 IFN-γ in animal models of systemic autoimmunity NIH-PA Author Manuscript Model (Strain) Disease IFN-γ Manipulation Disease Severity Reference CBAxC57/BL10 F1 SLE IFN-γ transgene Increased Seery, 2000 NZBW F1 SLE IFN-γ treatment Increased Jacob et al, 1987 Anti-IFN-γ treatment Reduced Jacob et al, 1987 Soluble IFN-γR Reduced Ozmen et al, 1995 IFN-γR null Reduced Haas et al, 1998 IFN-γR cDNA Reduced Lawson et al, 2000 IFN-γR null Reduced Hron & Peng, 2004 IFN-γR null Reduced Schwarting et al, 1998 IFN-γ null Reduced Balomenos et al, 1998 IFN-γR null Reduced Nguyen & Peck, 2013 IFN-γ null Reduced Nguyen & Peck, 2013 IFN-γR null Reduced Pollard et al, 2012 IFN-γ null Reduced Pollard et al, 2010 Spontaneous MRL-Faslpr NOD/ShiLtJ SLE SS Induced NIH-PA Author Manuscript Mercury (B10.S) SLE Pristane (BALB/cJ) SLE IFN-γ null Reduced Richards et al, 2001 Collagen (CFA)(DBA/1) RA IFN-γR null Increased Schurgers et al, 2011 Collagen (IFA) (DBA/1) RA IFN-γR null Reduced Schurgers et al, 2011 G6PI (CFA) (DBA/1) RA IFN-γR null Reduced Schurgers et al, 2011 NIH-PA Author Manuscript Discov Med. Author manuscript; available in PMC 2014 September 01.